Article
Which Stents Are Better: Drug-Eluting or Bare Metal?
Author(s):
Cardiologists have discussed the pros and cons of drug-eluting stents (DES) for several years. Some evidence seems to indicate that DES reduce risk of restenosis or ischemia-driven target vessel revascularization. They may, however, be more prone than bare metal stents to late (beyond 1 year) and sudden coronary artery occlusion.
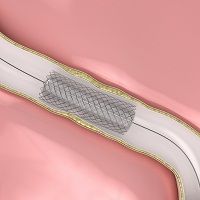
Cardiologists have discussed the pros and cons of drug-eluting stents (DES) for several years. Some evidence seems to indicate that DES reduce risk of restenosis or ischemia-driven target vessel revascularization. They may, however, be more prone than bare metal stents to late (beyond 1 year) and sudden coronary artery occlusion.
Researchers attribute this adverse event to DES’s inhibition of normal tissue growth. With bare metal stents, no inhibition occurs and normal tissue eventually coats their surfaces and inhibits blood clotting. If tissue fails to coat a DES, risk of sudden clotting may persist and create a prolonged need for dual antiplatelet therapy (DAPT).
Second-generation DES use different platforms, alternative drugs, and either more biocompatible durable polymers or bioabsorbable polymers. The November 2014 issue of Current Opinions in Cardiology reviews available evidence concerning second-generation stents in an article written by collaborators in the New York based Cardiovascular Research Foundation.
The authors find that recent data accruing from various types of meta-analysis challenge current beliefs that BMS are safer than DES. Among the evidence they review are several important findings:
- Cobalt-chromium everolimus-eluting stents (CoCr-EES) coated with durable fluorinated polymers may have significantly lower rates of stent thrombosis compared to other first and second-generation DES. They also seem to have lower rates of thrombosis than BMS.
- Four independent network meta-analyses suggest that CoCr-EES may have a better safety profile than bioabsorbable polymer-based DES.
- Fluoropolymers seem to exert a protective effect against stent thrombosis challenges.
- Second-generation DES have improved safety profiles and may reduce the need for prolonged DAPT
Progress has been steady in the field of stent development. Randomized controlled trials examining the new stents are needed, and once such trial (EXCEL) has already enrolled 1900 patients to percutaneous coronary intervention with CoCr-EES vs. coronary artery bypass grafting. The results are expected in 2016.





