Article
Why Do HCV Patients Report High Thyroid Dysfunction?
Author(s):
Elevated thyroid stimulating hormone was linked to female sex, higher BMI, liver fibrosis, AST, and low albumin.
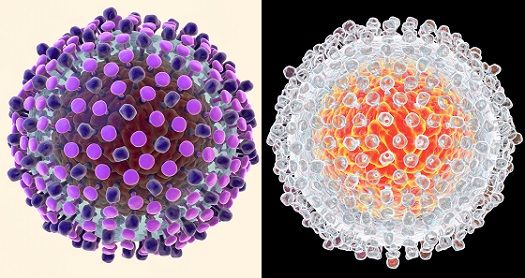
The most common extrahepatic endocrine and metabolic disorders diagnosed in patients with hepatitis C virus (HCV) are type 2 diabetes mellitus and thyroid dysfunction. Although the relationship between HCV and thyroid disorders is still be studied, HCV remains the only infectious agent entirely linked with autoimmune thyroiditis.
Those who are female, have genetic predispositions, borderline baseline TSH levels, or hypoechoic and small thyroid on ultrasounds, are more susceptible to thyroid dysfunction. Even among children with untreated HCV, the prevalence of thyroid dysfunction is higher than among children without HCV infection.
Rasha Eletreby, MD, a physician and researcher in the Department of Hepatology and Endemic Medicine at Cairo University in Egypt, led a retrospective study to evaluate the prevalence of thyroid dysfunction among patients with HCV.
A secondary aim of the study was to determine the potential impact of thyroid dysfunction on sustained virologic response (SVR) following treatment with direct-acting antivirals (DAAs).
The study included 13,402 patients with HCV genotype IV who were registered to receive HCV therapy through treatment centers affiliated with the National Committee for Control of Viral Hepatitis (NCCVH) through the Ministry of Health in Egypt, from January 2015 to October 2016.
All patients received DAA-based regimens. At the beginning of the study, some patients were still receiving interferon (IFN) therapy. However, IFNs were eliminated from treatment regimens once newer DAAs came to the market in Egypt. Demographic and clinical data were collected for all patients.
Of the 13,402 patients, 2833 (21.1%) had hypothyroidism, as indicated by elevated thyroid stimulating hormone (TSH) levels. Elevated TSH was significantly associated with female sex, higher body mass index (BMI), liver fibrosis, aspartate aminotransferase (AST), and low albumin.
Notably fewer patients (466, 3.5%) had low TSH levels, and the only variables associated were male sex and higher age. SVR was not found to be associated with baseline TSH levels.
A small cohort of patients (n= 236), for which follow-up TSH data was available, was analyzed to identify changes in TSH following SVR. Although the group was too small to draw any firm conclusions, all patients with elevated TSH prior to antiviral treatment experienced improvement in thyroid function following treatment.
Eletreby and colleagues noted that the biggest limitation of the study was a lack of follow-up TSH levels at end of treatment. This was likely due to the fact that treatment with DAAs, unlike IFNs, is not associated with inducing thyroid dysfunction, meaning such levels are not routinely measured in clinical practice.
Researchers concluded that hypothyroidism is prevalent in patients with chronic HCV GT4 — a factor heavily influenced by patients’ gender and age.
“We can also conclude that TSH level is not a predictor of response in the setting of direct acting antivirals,” researchers wrote. “On the other hand, SVR achievement after DAAs appears to improve thyroid dysfunction.”
The study, “High prevalence of HCV (GT4)-related TSH abnormality among 13402 Egyptian patients treated with direct acting antiviral therapy,” was published online in Hepatology International last month.
Click here to sign up for more MD Magazine content and updates.
Related Coverage >>>
Cytomegalovirus Reactivation Patients with HCV Cirrhosis Linked to Cardiovascular Risk





