Article
Wrist Pain in a 30-Year-Old Woman
She caught herself with her hands in a forward fall. A year later, her wrist is still painful. What should be done?
A 30-year-old woman who had an otherwise unremarkable medical history presented with a 1-year history of right wrist pain. The pain had started when she sustained a forward fall onto her right hand; it worsened when she moved the wrist or used that hand to lift or carry objects and was relieved with rest of the hand and wrist.
Physical examination revealed no external deformity. A ganglion cyst, 4 mm in diameter, was noted on the right dorsal wrist. Range of motion testing results were normal in both wrists. A scaphoid shift test was performed on both wrists; a positive result was seen on the right side.
Anteroposterior (AP) (left) and lateral (right) x-ray films obtained 1 year after the patient’s fall are provided here.


What do they show? What is your diagnosis?
Take a guess in the Comments box below.
Or move on to the next page for more information.
Wrist stability is maintained by the ligamentous interconnections between carpal bones and between the radius and carpus. When there is disruption of these ligaments, as in the case of this patient, wrist instability results.1
The scaphoid, along with its support mechanism, is the most vulnerable component of the wrist.2 If the ligamentous injury is incomplete, dynamic instability results. The carpal bones assume a normal alignment at rest but collapse under stress. When enough restraints are lost, static carpal instability results and the bones assume an abnormal alignment on standard wrist radiography.1
The most common form of carpal instability involves the scaphoid and the lunate. Generally, the mechanism of injury is a fall on an outstretched pronated hand (excessive wrist extension and ulnar deviation with intracarpal supination). The ligaments involved in scapholunate stability are the scapholunate interosseous ligament, the dorsal scapholunate ligament, and the volar radio- scapholunate ligament. It has been shown in anatomic studies that for dissociation to have occurred, 2 of the 3 ligaments must be disrupted.
When the scapholunate interosseous ligament is disrupted, the scaphoid assumes a flexed posture. Scapholunate dissociation alters articular contact areas and stress patterns with the carpus and leads to progressive degenerative arthritis of the wrist.1 The diagnosis of scapholunate ligament injury requires a high index of suspicion. Usually, patients recall a specific injury and present with dorsal, radial-sided wrist pain; loss of range of motion; and weakness of grasp.
Physical examination reveals tenderness over the scapholunate interval and a positive Watson scaphoid shift test result. In this test, the patient’s forearm is placed in pronation; the examiner places pressure on the volar distal pole of the scaphoid and the dorsal lip of the radius and moves the wrist from ulnar to radial deviation. A painful “clunk” with radial deviation and reproduction of the patient’s pain are considered positive test results;3 a clunk is not necessary for the result to be considered positive. Also, the test may not be accurate in an acute setting or in the presence of other injuries, such as a distal radial fracture. Wrist ganglia and carpal tunnel syndrome can be secondary manifestations of an underlying periscaphoid ligament injury.
Often, standard x-ray films reveal a flexed posture of the scaphoid and an extended lunate. On the AP x-ray view (below, right), the scaphoid appears foreshortened and results in an end-on view of the bone (the “cortical ring sign”). There is no separation of the scapholunate junction.2

Bilateral radiographic studies should be performed, including AP, lateral, radial and ulnar deviation, and clenched fist views, for comparison.1,4 Obtaining bilateral views is particularly important because many show a cortical ring sign on the asymptomatic side. A scapholunate gap is often visible;1 a separation of 3 to 4 mm or greater is significant for injury. Some authors consider a gap of more than 2 mm to be abnormal, especially if the gap is greater than that on the contralateral side.
Stress radiography (clenched fist view), including a grip view in full supination and an AP (supinated) view in maximum ulnar deviation, helps reveal scapholunate dissociation.5 If plain x-ray film results are normal and the index of suspicion is high, wrist MRI is the next study of choice, because it is both sensitive and specific.5
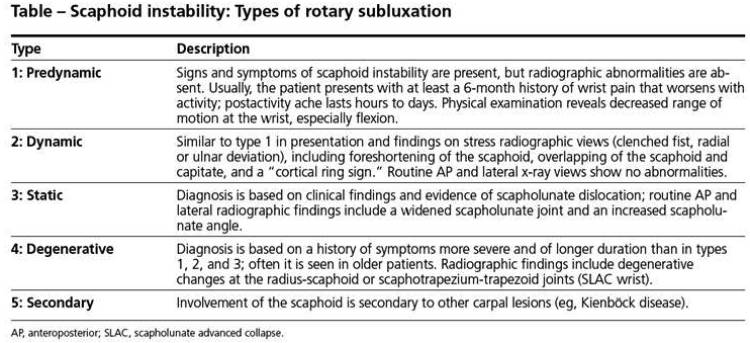
Use of fluoroscopy can provide evidence of dynamic instability, especially if symptoms are exacerbated by stress.4 If radiography does not provide evidence of rotatory subluxation of the scaphoid and conservative treatment has not succeeded, arthroscopy is indicated; some authors consider arthroscopy to be the gold standard of diagnostic imaging.4 Watson and associates2 described scaphoid instability as a spectrum of conditions that include 5 types of rotary subluxation of the scaphoid (see Tabl below).
As scaphoid instability progresses, clinical findings become more severe and radiographic findings become more apparent.
This patient’s ganglion cyst probably was related to the scapholunate injury. In this case, it was not a significant contributor of pain.
Initial treatment of acute scaphoid injuries with dynamic instability includes use of a short-arm cast with fingers and thumb free for 2 to 6 weeks, followed by a removable splint.
Gripping and weight-bearing exercises should be avoided. Gentle putty or sponge gripping can help improve grasp. Physical therapy modalities can be beneficial.5
Acute (less than 4 weeks) and subacute (4 weeks to 6 months) injuries of scapholunate dislocation with static instability should be managed operatively with open reduction and internal fixation because of the predictable arthritic changes that occur. Chronic injuries (more than 6 months) can be treated symptomatically with use of splinting and physical therapy modalities for joint protection.
Corticosteroid injections can help alleviate exacerbation of symptoms. If conservative management does not succeed, reconstructive or salvage procedures may be considered.1,5
Because these injuries are common and often missed and the decision about how to treat the patient is complex, primary care physicians, and even general orthopedic surgeons, often refer patients to the proper specialist, at least for consultation.
This patient was advised to have repeated radiography of the right wrist to evaluate the status of the scaphoid.Therapeutic options that were discussed included splinting as needed, physical therapy modalities and, possibly, joint injection.The patient declined repeated radiography and joint injection and opted for splinting and physical therapy.
This case was submitted by Marietta Babayev, MD, a specialist in physical medicine and rehabilitation practicing in South Charleston,West Virginia. It originally appeared in the May 2005 issue of the Journal of Musculoskeletal Medicine.




