Article
A Near Definitive Link Between Cigarette Smoke and Chronic Obstructive Pulmonary Disease
Author(s):
Patients with chronic obstructive pulmonary disease (COPD) often display inhibited mitochondrial protein pathways, according to a study published in the Journal of Clinical Investigation.
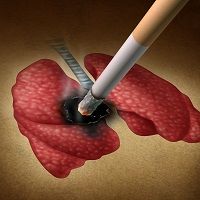
Patients with chronic obstructive pulmonary disease (COPD) often display inhibited mitochondrial protein pathways, according to a study published in the Journal of Clinical Investigation.
Researchers from Brown University examined healthy patients’ and smoking patients’ lung samples in order to demonstrate that the expression of the pathways in immune responses is decreased in COPD patients. The researchers examined the relationship between NLRX1, the protein known to inhibit the MAVS/ RIG-1-like helicase pathway, in the clinical stage of current and former smokers with COPD.
The team found that measured levels of the protein are a sign of cigarette induced emphysema, similar to the lung destruction that is seen in patients with COPD.
of thought in terms of what causes emphysema and a new school of thought regarding how cigarette smoke does what it does,” corresponding author and pulmonologist Jack A. Elias, MD, dean of medicine and biological sciences at Brown University, explained in a press release. “We’re showing that a lot of what's going on is related to mitochondria.”
Then, the investigators repeated a similar experiment in mice models. They were able to show a direct relationship between cigarette exposure, NLRX1, and the MAVS/ RIG-like helicase pathway. In this experiment, when the mice were exposed to smoke, they demonstrated lower levels of NLRX1 expression than the control mice which were not exposed. Mice that were biologically engineered to lack the gene for NLRX1 developed an advanced degree of emphysema when exposed to the cigarette smoke.
in the statement. “We observed that the levels of this molecule could explain diverse aspects of disease severity and patient’s symptoms.”
the MAVS/ RIG-like helicase pathway in the context of cigarette smoke exposure in both human and mice models.
tends to die down — but in human cases, it does not.
“We now have a common denominator that seems to bring all these hypotheses together,” Elias concluded. He added that single nucleotide differences in the protein’s gene may change a person’s susceptibility to COPD.






