Article
American Heart Association Issues Advisory on Oral Penicillin in Patients With High-Risk Rheumatic Heart Disease
Author(s):
The AHA released a statement related to use of oral penicillin for patients with high-risk rheumatic heart disease, including patients with severe mitral stenosis, aortic stenosis, left ventricular systolic dysfunction, or active symptoms of rheumatic heart disease.
This article was originally published on Practical Cardiology.
Amy E. Sanyahumbi, MD

In the wake of new research indicating some patients with rheumatic heart disease were dying from cardiovascular compromise following injections of benzathine penicillin G (BPG), the American Heart Association has released a presidential advisory to address the issue.
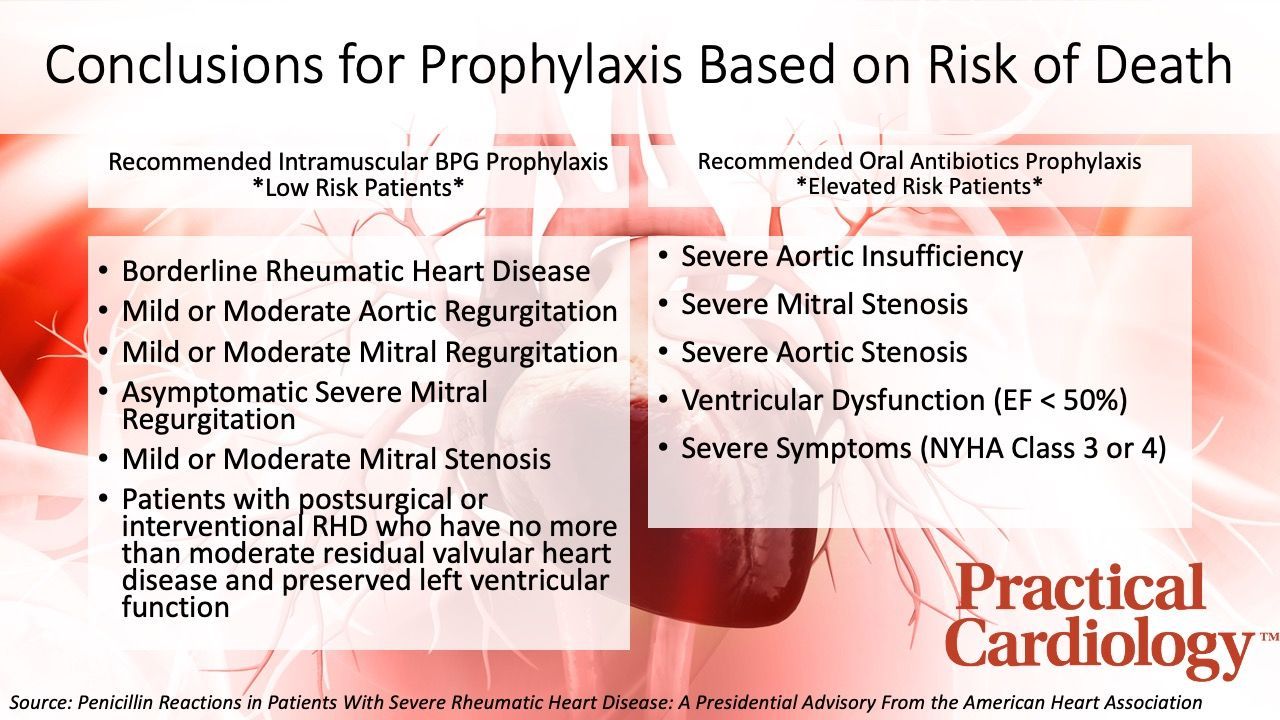
Published on January 20 with the intent of building awareness and providing strategies for risk reduction, the advisory from the AHA recommends oral penicillin, rather than BPG, for patients with high-risk rheumatic heart disease, which includes patients with severe mitral stenosis, aortic stenosis, left ventricular systolic dysfunction, or active symptoms of rheumatic heart disease.
”Until recently, deaths within the minutes and hours after BPG injection have been assumed to be due to anaphylaxis,” said Chair of the presidential advisory writing group Amy E. Sanyahumbi, MD, pediatric cardiologist at Texas Children’s Hospital and Assistant Professor of Pediatrics at Baylor College of Medicine, in a press release from the AHA. “However, a growing number of reports of BPG-related deaths did not have the features of classic anaphylaxis, and, instead, point to cardiovascular reactions. This distinction is important, as it indicates the need for different strategies to prevent or stop these reactions to BPG.”
An 8-page document with more than 3 dozen references, the presidential advisory was composed by Sanyahumbi and a team of 10 colleagues with the intent of raising awareness, providing risk stratification, and providing strategies for risk reduction. Using contemporary evidence, investigators developed criteria for stratifying patients as low risk and elevated risk of death from vasovagal compromise, which clinicians can use to determine which patients would benefit most from oral antibiotics as opposed to intramuscular BPG prophylaxis.
The statement from the AHA highlights multiple standard practices that should be followed by clinicians for patients receiving BPG. These include reducing injection pain and patient anxiety, ensuring patients are well-hydrated prior to injection, advising patients to eat a small amount of solid food within the hour before injection, the have patients receive the injection while laying down, and ensuring providers who administer BPG should be well-versed in recognizing and treating symptoms such as low blood pressure, low heart rate, or fainting.
“This advisory is urgently needed to raise awareness, provide risk stratification and guide health care professionals on easily implementable protocols to reduce risk and overcome reluctance to administer and receive BPG treatment for rheumatic heart disease,” said Andrea Z. Beaton, MD, vice-chair of the advisory writing group, a pediatric cardiologist at Cincinnati Children’s Hospital and associate professor of pediatrics at the University of Cincinnati School of Medicine.
This article, “Penicillin Reactions in Patients With Severe Rheumatic Heart Disease: A Presidential Advisory From the American Heart Association,” was published in the Journal of the American Heart Association.




