Publication
Article
Cardiology Review® Online
Appropriate Use and Clinical Impact of Transthoracic Echocardiography
Author(s):
Have the Appropriate Use Criteria for transthoracic echocardiography achieved their goal of having a significant clinical impact on physician decision making?
Karla K. Quevedo, MD
Review
Matulevicius SA, Rohatgi A, Das SR, Price AL, deLuna A, Reimold SC. Appropriate use and clinical impact of transthoracic echocardiography. JAMA Intern Med. [published online July 22, 2013] doi:10.1001/jamainternmed.2013.8972.
The increased use of all cardiac imaging services is affecting health care costs. Transthoracic echocardiography (TTE) is an available, easy-to-perform, and minimal-risk test, qualities that have made it one of the most frequently used cardiac imaging tests. Due to the increased demand of diagnostic imaging, the American Society of Echocardiography, in collaboration with the American College of Cardiology Foundation and other imaging subspecialty societies, developed guidelines for the Appropriate Use Criteria (AUC) for TTE. The AUC were initially published in 2007 and updated in 2011.
Study Details
Studies have shown that most TTEs are appropriate according to AUC for TTE, but the associations among TTE, AUC, and their clinical impact have not been well explored. Researchers from the University of Texas Southwestern Medical Center in Dallas reviewed a total of 617 TEE accounts from April 1 through April 30, 2011. A TEE was excluded from the review if there were not clinical data available to assign an AUC or if it was performed after cardiac transplant or implantation of a left ventricular assist device. Two general cardiologists reviewed all the electronic medical records before the TEE was performed and without knowing the results of the test and the clinical course subsequent to the performance of the TEE. The AUC was classified as appropriate, inappropriate, or uncertain as defined by the 2011 AUC. Two noninvasive cardiologists blinded to AUC classification independently assessed the clinical impact of each TEE after reviewing all the complete electronic medical data. Clinical impact was defined as (1) active change in care, (2) continuation of current care, or (3) no change in care. In further analysis, TTEs that led to active change were rated on a scale of 1 to 5 by consensus as very useful (5), useful (4), neutral (3), not useful (2), or misused (1) for affecting patient care. Any disagreements in clinical impact were resolved by consensus. If consensus could not be reached, a third blinded noninvasive cardiologist reviewed the cases and made a final assignment of clinical impact.
Differences in frequency distributions were statistically compared using the x2 test, and differences in continuous variables were compared using analysis of variance.
A total of 535 TEEs were included in the study. The percentage of female patients was 58.7%; 55.3% were white, 21.1% were African American, and 8.2% Hispanic, with a mean age of 58 years. Inpatient TEEs constituted 57.0% of all TEEs. Based on the 2011 AUC, 91.8% of TEEs were classified as appropriate, 4.3% as inappropriate, and 3.9% as uncertain. In the overall cohort, 31.8% of TEEs resulted in an active change in care, 46.9% led to continuation of current care, and 21.3% led to no change (Figure). In a more detailed analysis of the relative impact of active change, only 18.9% of all TEEs were classified as 5 (very useful) or 4 (useful) and 6.0% were classified as 2 (not useful) or 1 (misused) in affecting patient care. Cardiology as the ordering specialty was associated with a lower proportion of studies resulting in no change in care (12.6%) compared with pulmonary/ critical care and surgery (39% and 31.5%, respectively). There was no statistically significant difference between appropriate and inappropriate TEEs that led to active change in care (Figure).
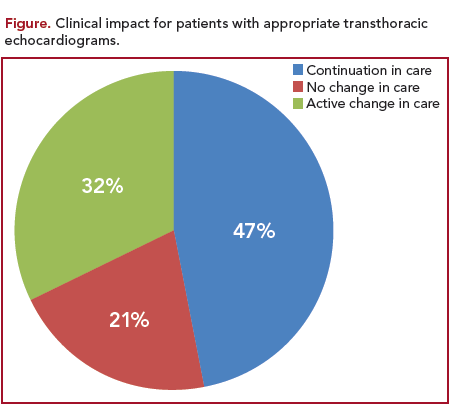
The study showed that although most TEEs (91.8%) were appropriate according to AUC, fewer than one-third of TEEs performed at a US academic medical center led to an active change in clinical care, nearly 50% resulted in a continuation of current care, and approximately one-fifth resulted in no change in care. The study reveals the large discrepancy between appropriateness and clinical impact. These alarming results suggest the need for changes in the current AUC guidelines in order to optimize the effective use of TEE.
CommentaryChange is Needed to Ensure Appropriate Use of TTE
Nowadays, transthoracic echocardiography (TEE) is one of the most commonly used noninvasive cardiac diagnostic tests. As reported by Medicare, TEE constitutes half of all cardiac imaging test ordered among beneficiaries,1 which translates to 11% and more than $1.1 billion of total diagnostic imaging spending in 2010.2
The latest updated AUC guideline for echocardiography was released in 2011. It specifically describes an “appropriate imaging study” as one in which the expected clinical judgment exceeds the expected negative consequences by a sufficiently wide margin for a specific indication and that the procedure is generally considered acceptable care and a reasonable approach for the indication.3 This publication classified 98 potential clinical indications as follows: appropriate (score of 7 to 9), uncertain (score of 4 to 6), and inappropriate (score 1 to 3).4 After the publication of the 2011 AUC guidelines, several studies assessed the application of these criteria in clinical practice. In general, studies that have evaluated the applications of AUC for TTE had similar results, with the vast majority of classifiable TTEs being ordered for appropriate indications (87% to 91%) and a smaller number classified as inappropriate (9% to 13%).5-7
The reason the American College of Cardiology and other subspecialty organizations created the AUC guideline is to impact physician decision making, healthcare delivery, and also reimbursement policy; in other words, reducing unnecessary healthcare expenditures but providing the best care for the patients. The aspect of cost cannot be avoided. An Institute of Medicine report found that 30% of healthcare spending in 2009—approximately $750 billion—was wasted, with $250 billion of that spent on unnecessary medical services.8 There is an urgent need for improvement in how medical resources are used—which will be achieved only if the number of unnecessary cardiac imaging tests are decreased.
Although a decrease in the number of inappropriate TTE has been reported since the publication of the 2011 AUC Guidelines, there is still room for improvement. Multiple strategies have been applied in order to decrease the number of inappropriate TTEs; one was the application of the 2011 AUC guidelines. Another strategy, used by Bhatia et al, was based on educational interventions including lectures to house staff on the 2011 AUC for TTE, the use of a pocket card that applied the AUC common clinical scenarios, and a biweekly e-mail feedback explaining the indication criteria for TTE. Using these simple educational interventions had a great impact on the reduction of the number of inappropriate TTEs ordered and in the increment of the proportion of appropriate TTEs ordered achieved at that inpatient academic medical center.9 Another proposed strategy to improve appropriate cardiac imaging test ordering is physician pre-screening, which has been shown to reduce inappropriate stress echocardiography orders.10 In the specific case of TTE, due to the high volume of studies, a prescreening strategy might not be practical. Although there is a better adherence to the AUC guidelines for TTE, TTE volume continues to increase year after year.
This interesting study by Matulevicius et al explores the association between AUC for TTE and their clinical impact. The study showed, as had previous studies, that 91.8% of the TTEs were appropriately indicated. However, the study showed another important perspective, not explored by many studies, which is that among the TTEs classified as appropriate, only 31.8% resulted in a change of care. The study found no statistically significant difference between appropriate and inappropriate TTEs in the number of TTEs that led to active change of care.
The study had several limitations, including the fact that the adjudication of clinical impact was done empirically and rated from 1 to 5 by consensus. This means that it was done according to the clinical experience of 2 noninvasive cardiologists, and in case of disagreement, a third cardiologist had to made a final assignment. A standard definition needs to be developed in order to assess clinical impact. Another limitation is that the study is retrospective and relies on electronic medical records; hence, incomplete or inadequate documentation can misclassify clinical impact or appropriate criteria. The study was performed in a tertiary care academic medical center, so the results cannot be generalized to other settings. The low prevalence of inappropriate TTEs limits the statistical power to detect a difference in the clinical impact between appropriate and inappropriate TTEs.
The data obtained in this study suggest that the main goal of the 2011 AUC guidelines for TTE have not been fulfilled: to have a significant clinical impact on physician decision making. The AUC working group stated that the definition of “imaging test appropriateness” must include an explicit understanding of how the test results might lead to care that could improve a patient’s morbidity and mortality. The study gives us a totally new perspective of the problem and also prompts more questions to be answered: do physicians recognize the right type of patient for whom to order a cardiac imaging test? When is the best time to order the test? How should the results be interpreted and used to have the greatest impact on patient health? Do the guidelines need to be both more detailed regarding appropriate criteria and establishing a clear definition of clinical impact? The need for research on this topic is evident, and understanding the role of echocardiography and its clinical contribution in patient management of each of the different pathologies is crucial. Until more data are available, the use and further update of the 2011 AUC guidelines should be a continuous process and its proper application by all physicians should be encouraged in inpatient and outpatient settings.
References
1. Perlman AS, Picard RT. Evolving trends in the use of echocardiography: a study of Medicare beneficiaries. J Am Coll Cardiol. 2007;49:2283- 2291.
2. Medicare Payment Advisory Commission. A data book: health care spending and the Medicare program. www.medpac.gov/documents/Jun- 12DataBookEntireReport.pdf. Published June 2012. Accessed August 30, 2013.
3. Douglas PS, Khandheria B, Stainback RF, et al. ACCF/ASE/ACEP/ASN/ SCAI/SCCT/SCMR 2007 appropriateness criteria for transthoracic and transesophageal echocardiography: a report of the American College of Cardiology Foundation Quality Strategic Directions Committee Appropriateness Criteria Working Group. J Am Coll Cardiol. 2007;50:187-204.
4. Douglas P, Garcia MJ, Haines DE, et al. ACCF/ASE/AHA/ASNC/ HFSA/HRS/SCAI/SCCM/SCT/SCMR 2011 Appropriate Use Criteria for Echocardiography. JACC. 2011;57:1126-1166.
5. Aggarwal NR, Wuthiwaropas P, Karon BL, et al. Application of the appropriateness criteria for echocardiography in an academic medical center. J Am Soc Echocardiogr. 2010; 23:267-274.
6. Willens HJ, Gomez-Marin O, Heldman A, et al. Adherence to appropriateness criteria for transthoracic echocardiography: comparisons between a regional Department of Veterans Affair health care system and academic practice and between physicians and mid-level providers. J Am Soc Echocardiogr. 2009;22:793-799.
7. Patil HR, Coggins TR, Kusnetzky LL, Main ML. Evaluation of appropriate use of transthoracic echocardiography in 1,820 consecutive patients using the 2011 revised appropriate use criteria for echocardiography. Am J Cardiol. 2012;109:1814-1817.
8. Institute of Medicine. Best care at lower costs: the path to continuously learning healthcare in America. http://www.iom.edu/~/media/Files/ Report%20Files/2012/Best-Care/Best%20Care%20at%20Lower%20 Cost_Recs.pdf. Published September 2012. Accessed September 24,2013.
9. Bhatia RS, Milford CE, Picard MH, Weiner RB. An educational intervention reduces the rate of inappropriate echocardiogram on an inpatient medical service. JACC: Cardiovascular Imaging, 2013;6:545-555.
10. Picano E, Pasanisi E, Brown J. A gatekeeper for the gatekeeper: inappropriate referral to stress echocardiography. Am Heart J. 2007; 154:285-290.
About the Author
Karla K. Quevedo, MD, is a Cardiology Fellow at Texas Tech University Health Sciences Center in El Paso, Texas. Dr. Quevedo received her MD at the Universidad San Martin de Porres in Peru. She was chief resident in internal medicine at Guillermo Almenara Hospital in Lima, Peru. Her areas of interest are general cardiology, preventive cardiology, and heart failure and biomarkers.






