Publication
Article
Family Practice Recertification
Basketball Player With Left Foot Pain
Author(s):
Slam dunking basketball player reports pain in his left foot and undergoes exams to determine the cause of the problem
James D. Collins, MD
History
This is a 22 year-old male basketball player that complained of left foot pain with difficulty walking after slam dunking basketballs. Examination by his coach detected mild swelling and tenderness over the outside of the left foot with discoloration over the region of the left fifth metatarsal bone suggesting a possible fracture. X-rays of his left foot were requested.
Radiographic Findings
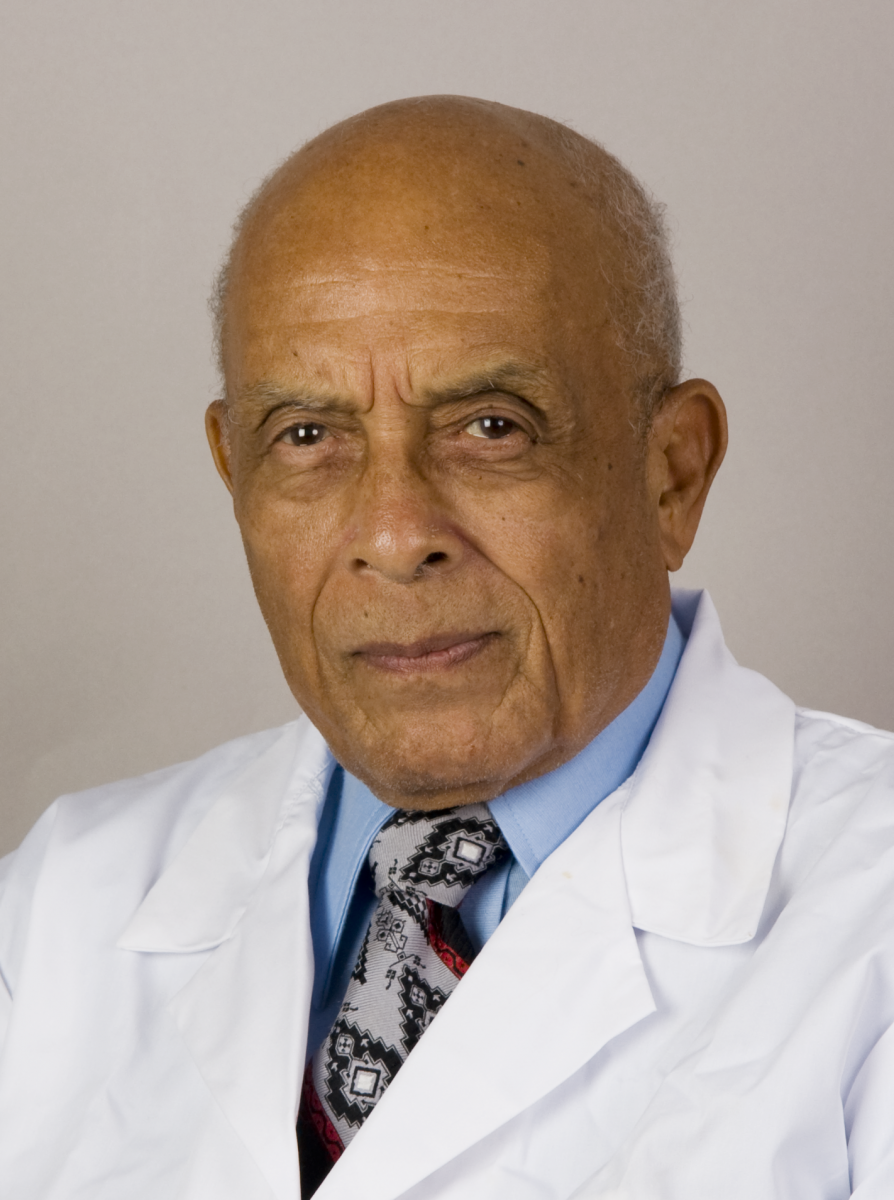
The lateral radiograph of the left foot (FIGURE 1) displays the disruption of the trabeculae within the tuberosity of the fifth metatarsal bone reflecting the fracture (FX) site. Figure 1 was inverted (FIGURE 2) to give a different perspective to the enlarged radiograph of the left foot to best display the disrupted trabeculae of the left fifth metatatarsal bone. Figure 3 is a cone-down oblique radiograph displaying the fracture site with marginating landmark anatomy. Figure 4 is an enlarged lateral radiograph of left foot to enhance the fracture site and landmark anatomy of the left foot.
The images can be compared to a normal x-ray of a foot and ankle to better appreciate the osseous structures (2). The reader should understand that an x-ray displays only 70% of the anatomic structures because 30% of the x-ray beam is absorbed by structures imaged. The images selected for this case were enlarged and inverted to better display the landmark anatomy.
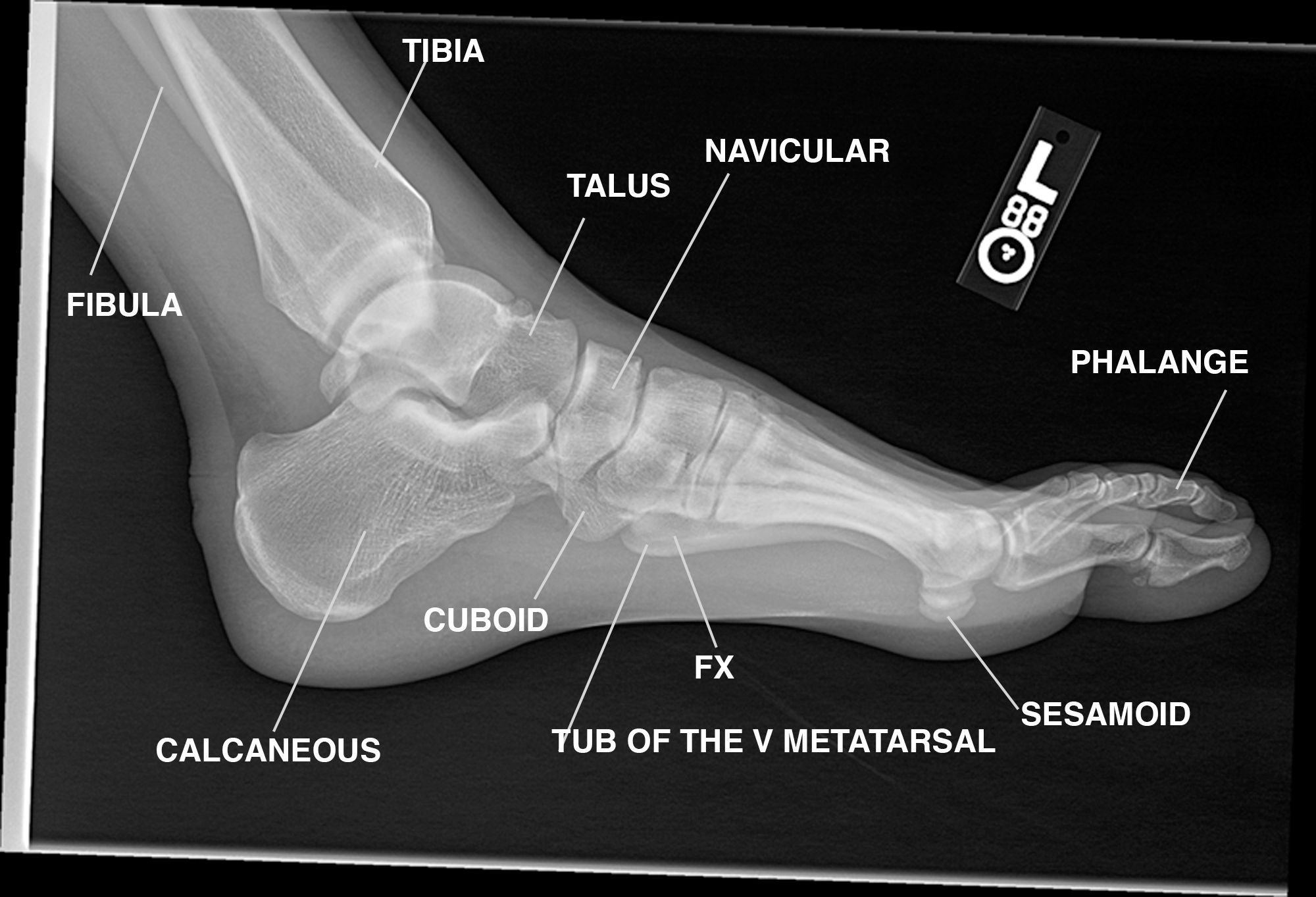
FIGURE 1 is the left lateral non-weight bearing annotated x-ray of the left foot. Observe the fracture site of the tuberosity of the fifth metatarsal bone (TUB OF THE V METATARSAL), Fracture (FX) of the disrupted trabeculae in the fifth metatarsal bone. Left (L).
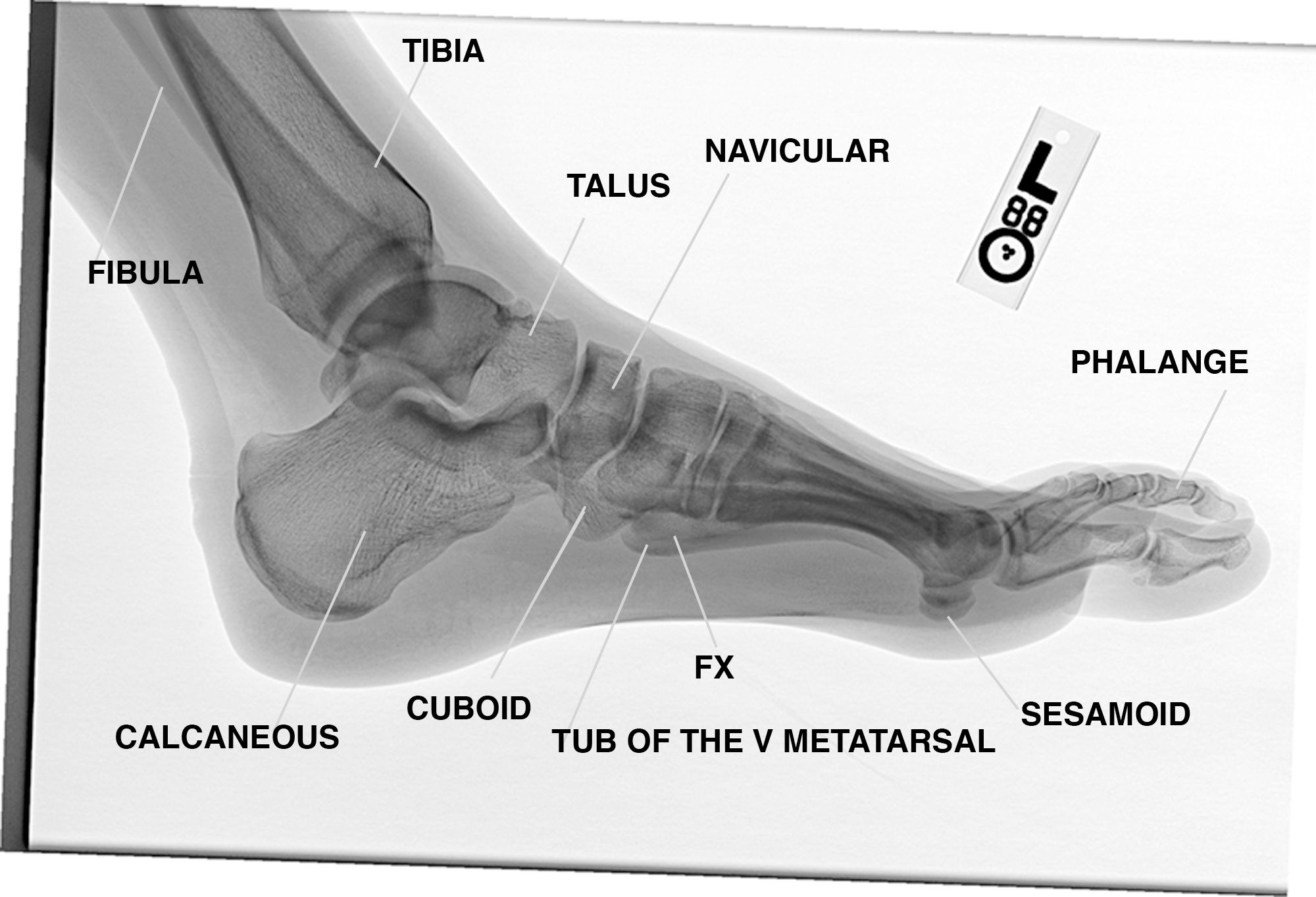
FIGURE 2 is the inverted left lateral none weight bearing annotated x-ray of the left foot. Observe the fracture site of the tuberosity of the fifth metatarsal bone (TUB OF THE V METATARSAL), Fracture (FX) of the disrupted trabeculae in the fifth metatarsal bone.
Left (L).
FIGURE 3 is the cone down oblique radiograph of the fracture site displaying disruption
Of the trabeculae by the fracture (FX).
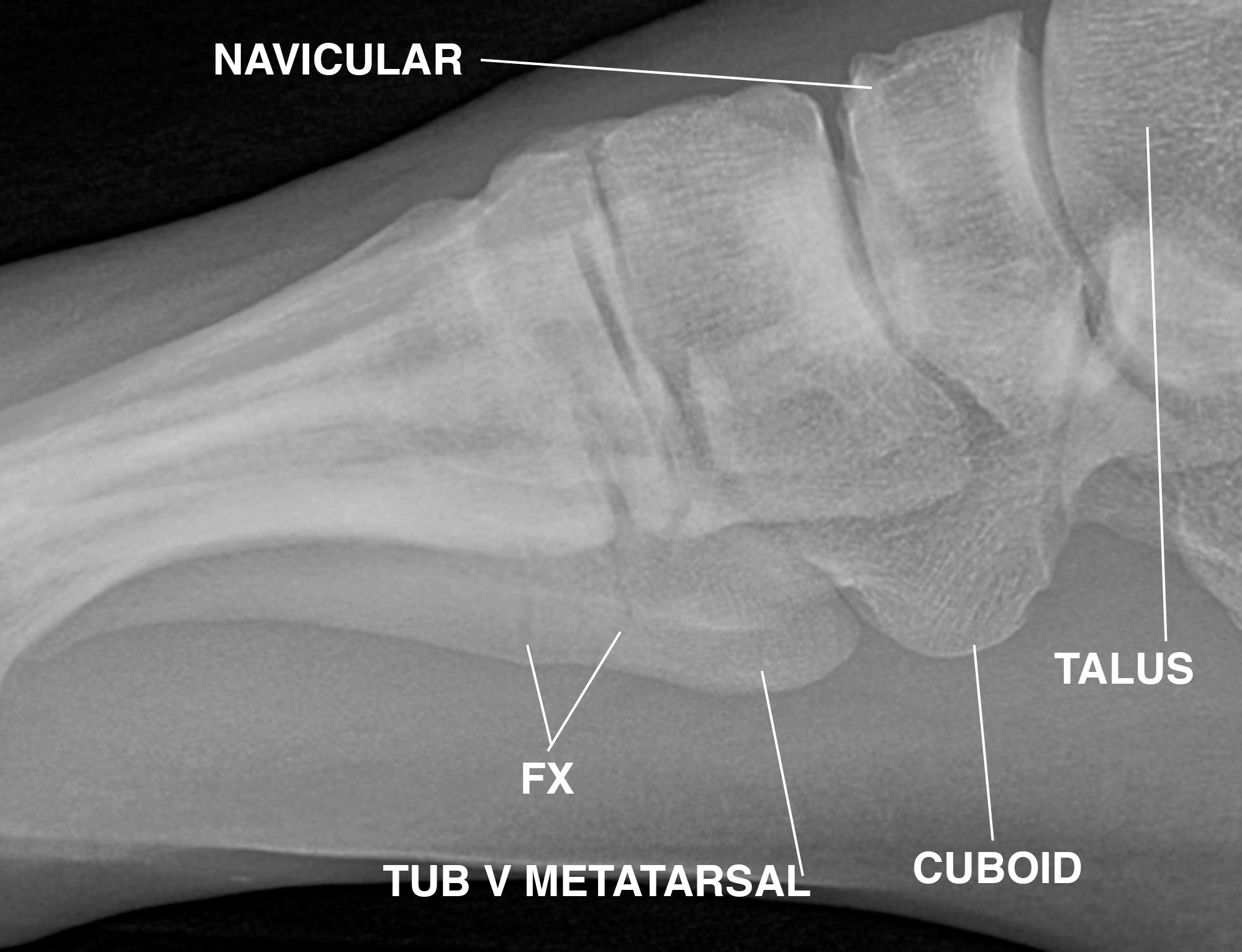
FIGURE 4 is the left lateral enlarged non-weight bearing image of FIGURE ONE.
Discussion
The fifth metatarsal bone is a long bone in the foot. It is the second smallest of the five metatarsal bones. The fifth metatarsal is analogous to the fifth metacarpal bone in the hand [1, 2]
The metatarsal bones are divided into three parts; a base, body and head. The base is the part closest to the ankle and the head is closest to the toes. The narrowed part in the middle is referred to as the body, or shaft, of the bone. The bone has two flattened surfaces; the plantar and the dorsal surface. The surfaces are roughened for ligamentous attachments. The bone is curved in length, concave inferiorly, and slightly convex superiorly (2).
The bases are smooth and articulate proximally, with the three cuneiform bones and the cuboid bone having articular groves for facets on their sides. The fifth metatarsal has a rough eminence, the tuberosity, on the lateral side of its base. The plantar surface of the base is grooved for the tendon of the abductor digiti quinti.
(2)
The head articulates with the fifth proximal phalanx, the first bone in the fifth toe. The plantar aponeurosis connects the tuberosity with the lateral process of the tuberosity of the calcaneus. (1, 2)
The base of the metatarsal is often injured as a Jones fracture. When the fracture involves the tuberosity, , it is called a pseudo-Jones fracture. This is a common fracture of the fifth metatarsal.[3] A Jones fracture occurs slightly distal in a small area of the fifth metatarsal that receives less blood and is therefore more prone to injury. These fractures can be either a stress fracture, a tiny hairline break that occurs over time, or an acute or sudden break as in our athlete. The Jones fractures are caused by overuse, repetitive stress, or trauma. They are less common and more difficult to treat than avulsion fractures. Because a Jones fracture sometimes does not show up on initial x-rays, additional imaging studies may be needed (3, 4).
Unlike most metatarsal stress fractures which do not require immobilization or casting, stress fractures of the proximal 5th metatarsal are at increased risk for delayed union and non-union. Rest is crucial and patients should be advised to stay off the injured foot, since walking can cause further damage. Ice may be applied to reduce swelling and pain, A bag of ice may be applied over a thin towel to the affected area for 20 minutes of each waking hour. Ice should not be directly applied on the suspected fracture site. Crutches should be provided and the importance of strict non-weightbearing should be emphasized to the patient. Orthopedic consultation is indicated.
Take-home Message
Stress fractures involving the 5th metatarsal are at high risk for non-union. Unlike other metatarsal stress fractures, these fractures require strict immobilization and orthopedic consultation. Annotated landmark anatomy is important in making an accurate diagnosis. A diagnosis may be made from a single plain X-Ray radiograph. However, osseous and soft tissues are not well displayed on x-rays because 30% of an x-ray beam is absorbed by the tissue with 70% of the x-ray beam responsible for the image displayed. Follow-up radiographs should be obtained to define the healing process.
References
1) CARMINE D. CLEMENTE, Anatomy, A Regional Atlas of the Human Body, Fifth Edition p 450-451.
2. Woodburne RT, Burkel WE. (1988.) Essentials of Human Anatomy. (8th ed.). New York: Oxford University Press.
3. http://www.foothealthfacts.org/footankleinfo/fifth-metatarsal_fractures.htm
American College of Foot and Ankle Surgeons
4. Wheeless' Textbook of Orthopaedics, http://www.wheelessonline.com/ortho/jones_fracture
About the Author
James D. Collins, MD, is Professor and General Radiologist in the Department of Radiology at the UCLA David Geffen School Medicine. He formerly served as Director of the required medical student training for the department and President of the James T. Case Radiologic Foundation.
Collins has an extensive background of publications, consultations, and editorial positions, including his current post as the Radiology Editor for the Journal of the National Medical Association. He specializes in bilateral 3-dimensional MRI and MRA imaging of the brachial plexus and has been performing those studies since 1985.






