Article
Cardiology Case Report: Return of Spontaneous Circulation
Author(s):
Our latest cardiology case report features a man in his mid-70s with a history of COPD and laryngeal cancer brought in after a week of worsening generalized weakness and DOE without fever, pain, or other complaints. Can you determine the correct diagnosis?
History:
A patient in their mid-70’s with a history of COPD and laryngeal cancer is brought to the hospital for cardiac arrest. Medics state the call went out for 1 week of worsening generalized weakness and DOE without fever, pain or other complaints. He was initially alert but once loaded into the rig became unresponsive and pulseless. With about 1 minute of CPR they got pulses back. The initial rhythm was PEA. No shocks or medications were given. The patient is lethargic but denies palpitations, chest pain, leg swelling or pain, fever, cough or other complaints.
Exam:
Heart rate is about 125, BP is in the 80’s. The patient is a bit lethargic
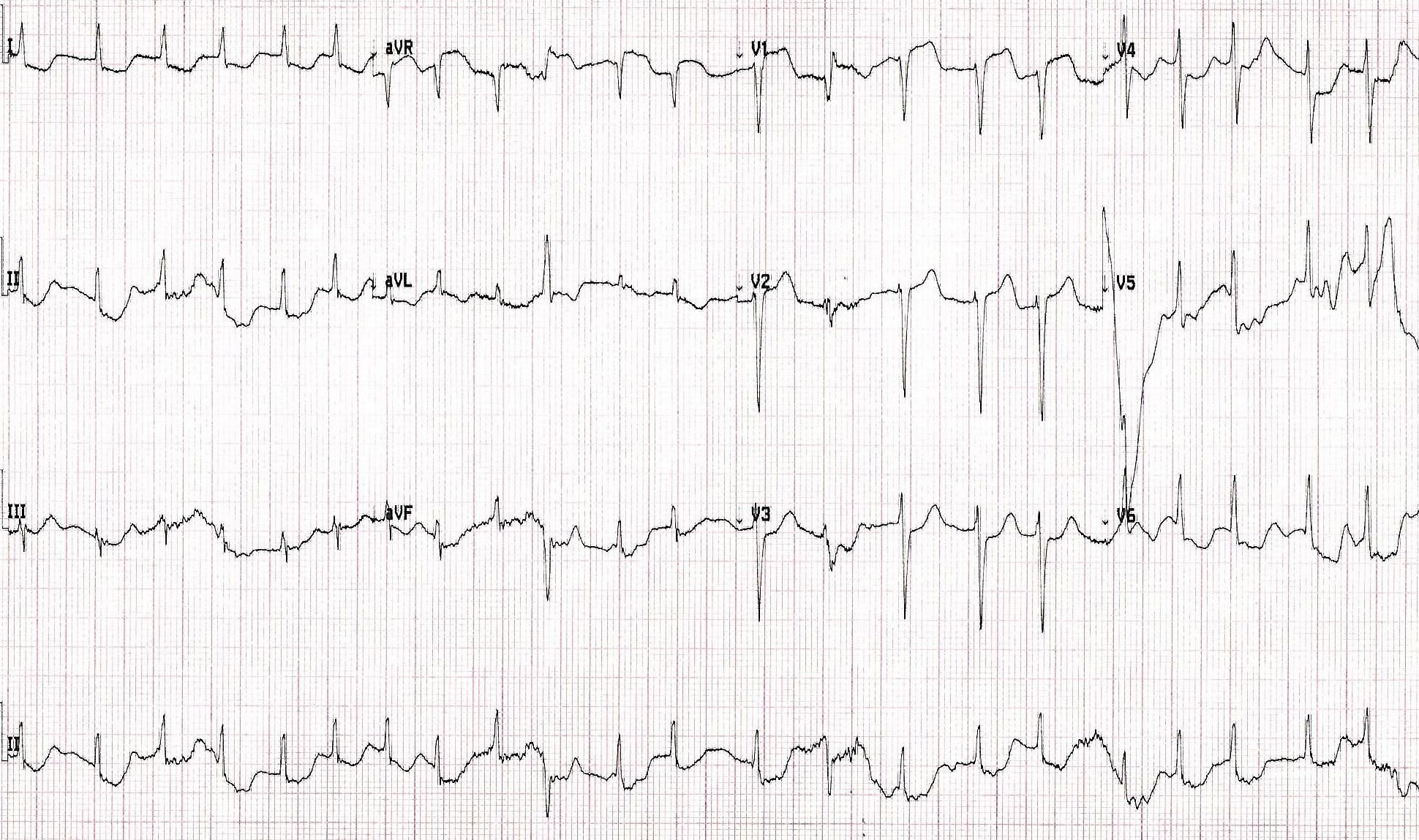
An ECG is done
Computer Read: atrial fibrillation with RVR at 139, marked ST depression – consider subendocardial injury ***ACUTE MI****
Other info: a bedside echo was done. COPD limited quality of parasternal view but the subxiphoid view showed a dilater right ventricle.
Soon after arrival he has another PEA arrest.
What is the most likely cause of the ECG findings in this patient?





