Publication
Article
Cardiology Review® Online
Change in Readmissions and Follow-up Visits as Part of a Heart Failure Readmission Quality Improvement Initiative
Author(s):
Do mandatory follow-up visits after discharging heart failure patients decrease rehospitalizations?
Karla K. Quevedo, MD
Review
Am J Med.
Ryan J, Kang S, Dolacky S, Ingrassia J, Ganeshan R. Change in readmissions and follow-up visits as part of a heart failure readmission quality improvement initiative. 2013;126:989-994.
Study Details
One of the strategies to decrease the incidence of rehospitalization in patients with heart failure (HF) is the implementation of a mandatory follow-up visit early after discharge. Data has been discrepant, with some studies indicating benefit of outpatient follow-up1 and some indicating lack of benefit.2 The objective of the present study was to quantify the impact of 7-day follow-up visits and 30-day readmission rates as part of a hospital quality improvement initiative and to characterize events at 7-day follow-up visits.
International Classification of Diseases, Ninth Revision
The study was single-center and retrospective. It compared the data of 1 year before and 1 year after (2009 and 2010) the heart failure readmission quality improvement initiative. The primary outcomes after the implementation of outpatient visits were: change in 30-day all-cause readmission rates for HF and change in number of the University of Connecticut (UCONN) Health Center 7-day follow-up visits. The determination of 30-day all-cause readmission rate was obtained from the Connecticut Hospital Association ChimeData database, which contains all hospitalizations within the state of Connecticut. An inclusion criterion was to have a primary diagnosis of HF based on the , diagnosis code. Exclusion criteria were any patients that were transferred to another hospital, patients that died in the hospital, or patients who left against medical advice. A readmission was defined as a hospitalization for any reason within 30 days after discharge, and only the first readmission was counted in case of multiple readmission in the 30-day period. A total of 398 charts were reviewed in the study.
z
The quality improvement interventions used were: pre-discharge education, timely mandatory follow-up visits 7 days after discharge, and coordination of services with the community providers. Demographic and clinical variables were obtained from the charts. Statistical analysis was performed using SAS 9.3 (SAS Institute Inc, Cary, North Carolina). For comparison of the change in readmission rate and number of 7-day follow-ups, a 1-sided test was used. The level of statistical significance was set at .05.
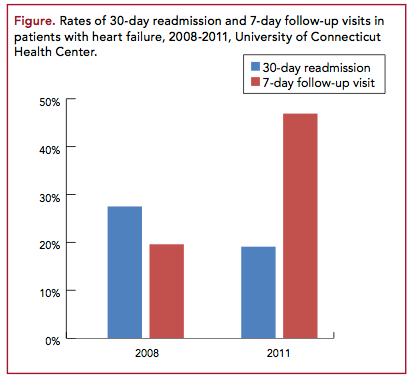
The results of the study indicated a reduction in the HF 30-day readmission rate from 27.5% in 2008 to 18.1% in 2011 after implementation of the quality improvement initiative. This represents an absolute decrease of 30%. There was an increment in the frequency of 7-day follow-up visits from 10.6% in 2008 to 46.9% in 2011 (Figure 1). All of the outpatient follow-up visits considered in the study were
performed at UCONN Heart Failure Center. Visits at UCONN tended to occur 3 to 7 days after discharge and were performed mainly by a cardiologist or an HF advanced practice registered nurse. The most common medications changed were diuretics. Five patients had a new diagnosis at the follow-up visit that was not present at discharge. Three patients required intravenous diuretics at follow-up visit. Discrepancies between discharge medications and follow-up medications were common: 21% of patients were missing a cardiac medication at follow-up visit that was not listed at hospital discharge, 2% of patients were taking cardiac medications at follow-up that was not listed at discharge, and 25% of patients had a cardiac dose discrepancy between discharge and follow-up visit.
Limitations of the study include the lack of a control group, so any causality between the decrease in readmission rates and any of the 3 components of the quality initiative could not be determined. The follow-up visits included in the study were performed at UCONN, so the readmission rates among patients with and without follow-up visits could not be compared due to possible missed follow-up visits in another institution. Other limitations include this study being a single-center study, so the findings cannot be generalized to other hospitals of different capacity, and the fact that readmissions were determined just within the state of Connecticut, so it is possible that there were missed readmission data outside the state.
The study showed that the implementation of a 7-day follow-up visit as part of a quality improvement program for HF readmission was successful. The investigators also made some important observations. Many of the readmitted patients were seen within 7 days, indicating that the follow-up visit did not prevent readmissions in all cases. The evidence of new diagnoses found at the follow-up visit could indicate that many patients with HF within 1 week of discharge are not completely medically stable. As shown in prior studies, the medication discrepancies between discharge and follow-up visits were very common; it correlates with the large number of medications on which this population must be maintained (average, 9 daily medications for this study). Although some studies have suggested that follow-up by a cardiologist could improve outcomes, type of provider at follow-up did not change the outcomes in this study.
CommentaryAre 30-day Rehospitalization Rates Even an Accurate Marker of Health-System Quality?
T
he cost of health care in the United States is growing more rapidly than national incomes. Health expenditures for 2013 consumed nearly 18% of the gross domestic product.3 The Centers for Medicare & Medicaid Services identifies readmission of patients within 30 days of discharge as a quality metric.4,5 Although the 30-day period is arbitrary, it represents an important preexisting time in quality outcome in oncology, cardiac surgery, and HF management.6 HF represents the most common cause of hospitalization in elderly patients, resulting in 6.5 million hospital days in the United States annually.7 It is crucial to have a good understanding of the physiopathology, classification, and management of HF in order to implement strategies to decrease readmissions rate and reduce hospitalization costs.
HF is a complex entity that can manifest with cardiac and noncardiac abnormalities. A distinction should be made between outcomes in outpatients with chronic HF and patients with hospitalization for HF (HHF). In chronic HF, prognosis has significantly improved since the advent of new therapies and devices. Patients with HHF continue to have a high mortality and readmission rates that have not improved in the last 2 decades despite new therapies.8 In the EVEREST (Efficacy of Vasopressin Antagonism in Heart Failure Outcome Study with Tolvaptan) trial, 24% of HHF patients were readmitted within 30 days of discharge.9 In the OPTIMIZE-HF (Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure) registry, rates of rehospitalization were 30% at 60 days post discharge.10 Precipitants for HHF include cardiac factors, noncardiac factors, patient-related factors, dietary indiscretion, drug and alcohol abuse, iatrogenic factors, and system-related factors, like poor transitions of care.11,12 Each of these factors could be used as a possible target in order to prevent readmissions. Multiple strategies to decrease readmission rates have been studied. Koelling et al reported that a 1-hour nurse-conducted teaching session at discharge resulted in improved clinical outcomes.13 Recently updated American Heart Association performance measures for HHF patients included follow-up outpatient visit (within 7 to 14 days) and early telephone follow-up as reasonable recommendations.14,15 This study by Ryan and colleagues shows that addressing some of the precipitant factors for HHF can have an impact on decreasing 30-day readmission rates, as shown in other studies.
Finally, multiple studies have shown that 30-day rehospitalization is not associated with better performance on quality measures, or 30-day mortality risk. Hospitals with the shortest rates of 30-day readmission, paradoxically, performed worse on HF core measures.16 Based on this evidence, the use of 30-day rehospitalization rates remains controversial as an accurate marker of health-system quality. More trials are needed to better understand the course of HHF leading to readmission and to investigate interventions that lead not just to fewer hospitalizations or lower costs but mainly to better outcomes.
References
1. Coleman E. The post-hospital follow-up visit: a physician checklist to reduce readmissions. Oakland, CA: California HealthCare Foundation Issue Brief; October 2010.
Arch Intern Med
2. Grafft C, McDonald K, Ruud J, et al. Effect of hospital follow-up appointment on clinical event outcomes and mortality. . 2010;170:955-960.
Health Affairs
3. Keehan SP, Cuckler GA, Sisko AM, et al. National health expenditure projections: modest annual growth until coverage expands and economic growth accelerates. . 2012;31:1600-1612.
JAMA
4. Joynt KE, Jha A. Characteristics of hospitals receiving penalties under the hospital readmissions reduction program. . 2013;309:342-343.
N Engl J Med
5. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. . 2009; 360:1418-1428.
JAMA
6. Vaduganathan M, Bonow RO, Gheorghia de M. Thirty-day readmissions: the clock is ticking. . 2013;309:345-346.
J Am Coll Cardiol.
7. Hunt SA, Abraham WT, Chin MH, et al. 2009 focused update incorporated into the ACC/AHA 2005 guidelines for the diagnosis and management of heart failure in adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. 2009;53:e1-e90.
J Am Coll Cardiol.
8. Gheorghiade M, Vaduganathan M. Rehospitalization for heart failure: problems and perspectives. 2013;61:391-403.
Am Heart J
9. O’Connor CM, Miller AB, Blair JE, et al. Causes of death and rehospitalization in patients hospitalized with worsening heart failure and reduced left ventricular ejection fraction: results from Efficacy of Vasopressin Antagonism in Heart Failure Outcome Study with Tolvaptan (EVEREST) program. . 2010;159:841-849.
J Am Coll Cardiol
10. Fonarow GC, Stough WG, Abraham WT, et al. Characteristics, treatments, and outcomes of patients with preserved systolic function hospitalized for heart failure: a report from the OPTIMIZE-HF registry. 2007;50:768-777.
JAMA.
11. Gheorghiade M, Braunwald E. A proposed model for initial assessment and management of acute heart failure syndromes. 2011;305:1702-1703.
Heart Failure Clin
12. Psotka MA. Strategies to prevent post-discharge adverse events among hospitalized patients with heart failure. . 2013;9:303-320.
Circulation
13. Koelling TM, Johnson ML, Cody RJ, Aaronson KD. Discharge education improves clinical outcomes in patients with chronic heart failure. . 2005;111:179-185.
. J Am Coll Cardiol.
14. Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: executive summary 2013;62:e147-e239.
J Nurse Pract.
15. Kim SM, Han HR. Evidence-based strategies to reduce readmission in patients with heart failure. 2013;9:224-232.
Am Heart J.
16. Kociol RD, Liang L, Hernandez AF. Are we targeting the right metric for heart failure? comparison of hospital 30-day readmission rates and total episode of care inpatient days. 2013;165:987-994.
About the Author
K
arla
K. Q
uevedo
, MD,
is a Cardiology Fellow at Texas Tech University Health Sciences Center in El Paso, Texas. Dr Quevedo received her MD at the Universidad San Martin de Porres in Peru. She was chief resident in internal medicine at Guillermo Almenara Hospital in Lima, Peru. Her areas of interest are general cardiology, preventive cardiology, and heart failure and biomarkers.






