Publication
Article
Internal Medicine World Report
Closing the Postherpetic Neuralgia Treatment Gap in Primary Care
Author(s):
Noting the management and treatment of postherpetic neuralgia (PHN) are currently subpar in the primary care setting, 2 researchers recently reviewed and outlined key clinical considerations for the chronic neuropathic pain syndrome.

Noting the management and treatment of postherpetic neuralgia (PHN) are currently subpar in the primary care setting, 2 researchers recently reviewed and outlined key clinical considerations for the chronic neuropathic pain syndrome in the Journal of Pain Research.
Beginning with the etiology of PHN, Jamie S. Massengill of JSM Medical in Edmond, OK, and John L. Kittredge of Michiana Spine, Sports & Occupational Rehab in Mishawaka, IN, described how the chronic pain condition is a common complication of herpes zoster (HZ), or shingles, caused by the reactivation of varicella zoster virus (VZV). PHN is predominantly diagnosed in patients aged 60 years or older who have recovered from HZ’s hallmark painful skin rash, yet continue to experience pain in that region for at least 3 months, the reviewers added.
“For primary care providers, PHN may not present as a distinct entity, but rather an extension of the original herpes zoster (HZ) infection, and monitoring for a global condition affecting multiple aspects of patients’ lives, rather than for a localized post-HZ pain is paramount,” the authors explained. “Thus, the practical management of PHN can be divided into prevention and treatment of HZ, and the more challenging task of managing the neuropathic pain syndrome and its consequences once PHN has developed.”
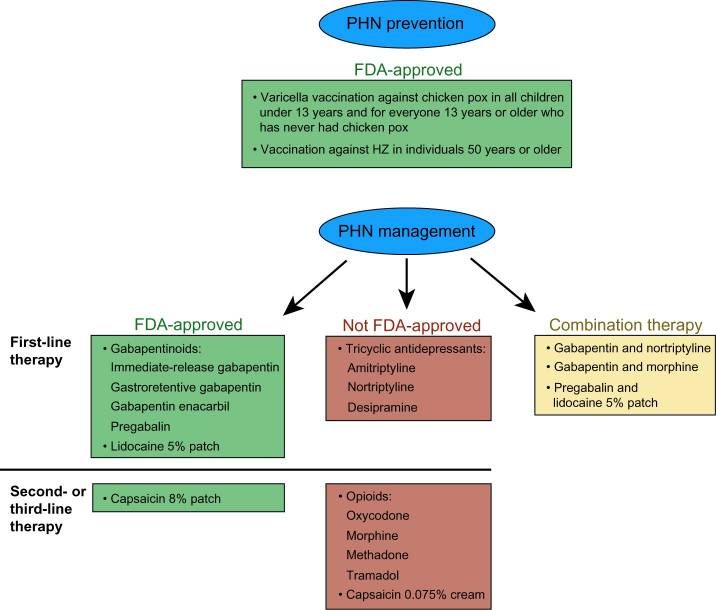
In terms of preventative measures, Massengill and Kittredge said the widely available varicella and VZ vaccines inhibit initial VZV infection and subsequent HZ, but they “remain widely underused, mainly due to the surprising lack of vigilant recommendation by primary care providers, as well as lack of awareness of HZ and the HZ vaccine.”
Considering the unsatisfactory prevention of PHN, the authors advised clinicians to develop a “carefully devised, individually based treatment plan to ensure optimal outcomes in the management of PHN.” Since no single treatment is capable of addressing all of the condition’s underlying complex pain mechanisms, the reviewers said “the initial choice of PHN pain therapy should be guided not only by drug efficacy, but also by the patient’s comorbidities, severity of PHN pain, the drugs’ adverse-event and drug-interaction profiles, titration regimen, and patient preference.”
Such first-line treatment choices might include oral therapies like gabapentinoids, topical therapies like the lidocaine 5% patch, or a combination of both types, which would more effectively “target multiple sites along the PHN pain pathway (and) result in better analgesia,” the authors wrote.
Despite those accessible therapeutic options, PHN treatment is “often inadequate, leaving patients undertreated,” Massengill and Kittredge noted. To close that treatment gap, they recommended “better utilization of available options and multimechanistic approaches to PHN management based on the patient’s individual characteristics.”
“Primary care plays a crucial role in the development and implementation of the PHN treatment plan, and establishing effective communication with patients,” the authors concluded. “Well-devised and well-executed PHN therapy will not only ensure sufficient pain relief, but will also facilitate improvements in patients’ physical and psychosocial functions.”






