Article
CNS Vasculitis: A Protean Manifestation of HIV/AIDS
A 42-year-old Hispanic woman with a past medical history of HIV infection and noncompliance with highly active antiretroviral therapy was admitted to the emergency department with a new-onset generalized tonic-clonic seizure episode, followed by Todd paralysis.
ABSTRACT: A woman with a past medical history of HIV infection and noncompliance with highly active antiretroviral therapy (HAART) was admitted with a new-onset generalized tonic-clonic seizure episode, followed by Todd paralysis. Physical examination demonstrated slurred speech and 4/5 muscle strength on the patient's right leg and arm; she was lymphopenic. Antiepileptic treatment was started, and the patient was referred to the HIV clinic for reinitiation of HAART. Magnetic resonance angiography of intracranial circulation was performed using 3-dimensional time of flight technique; the findings were consistent with probable HIV vasculitis. The majority of HIV-associated vasculitic disorders occur in the state of advanced infection. In suspected vasculitis, searching for cryoglobulinemia and drug-induced angiitis is especially important. There are several possible drug associations. (J Musculoskel Med. 2011;28:462-464)
A 42-year-old Hispanic woman with a past medical history of HIV infection and noncompliance with highly active antiretroviral therapy (HAART) was admitted to the emergency department with a new-onset generalized tonic-clonic seizure episode, followed by Todd paralysis. In this case report, we describe a CNS disorder in this patient caused by HIV-associated vasculopathy.
Case presentation
Physical examination demonstrated slurred speech and 4/5 muscle strength in the patient's right leg and arm. She was lymphopenic, with a peripheral CD4+ cell count of 44/μL. Antiepileptic treatment with phenytoin and levetiracetam was started, and the patient was referred to the HIV clinic for reinitiation of HAART and preventive treatment for opportunistic infections. At a follow-up appointment with the HIV service after 3 months of HAART, the patient's CD4+ cell count had increased to 300/μL, and she had no recurrence of the neurological manifestations.
Imaging
Magnetic resonance angiography (MRA) of intracranial circulation was performed using 3-dimensional time of flight technique. Shown were narrowing and luminal irregularity of the bilateral anterior, middle, and posterior cerebral arteries (Figure 1, double-arrows) and a high-grade obstruction of the distal M1 segment of the left middle cerebral artery (Figure 1, single arrow). The obstruction might account for the cortical and subcortical edema identified in fluid-attenuated inversion-recovery images of the left hemisphere (Figure 2, arrow). These findings were consistent with probable HIV vasculitis.
Diagnosis of exclusion
A CNS disorder caused by HIV-associated vasculopathy is a diagnosis of exclusion. The majority of HIV-associated vasculitic disorders occur in the state of advanced infection. Vasculitides are a rare but major manifestation of HIV infection, with an incidence of less than 1%, excluding adverse drug reactions. They may result from HIV-accompanying infections (hepatitis B and C virus, varicella zoster virus, cytomegalovirus infections) or from a direct infection of vascular or perivascular tissue by HIV.1 In our patient, the serology results for viral infections, other than HIV, were negative.
FIGURE 1
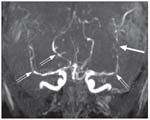
Magnetic resonance angiography of intracranial circulation
As part of the immunocompromise caused by HIV, a granulomatous inflammation that involves small arteries and veins of the brain surface and leptomeninges, termed a “primary angiitis of the CNS,” is a rare vasculitis associated with a high rate of mortality. None of the systemic vasculitides that may have CNS manifestations was present in this patient.
In suspected vasculitis, searching for cryoglobulinemia and drug-induced angiitis is especially important. Possible drug associations include thiouracil, allopurinol, minocycline, D-penicillamine, carbamazepine, phenytoin, methotrexate, and isotretinoin. However, our patient was not receiving any of these drugs, and the results of tests for hepatitis C and cryoglobulinemia were negative.
MRI findings characteristic of CNS vasculitis in patients with HIV infection include white matter changes, multiple cavitary infarcts, thrombus formation, stenosis, and microaneurysms of the large cerebral vessels. Three types of vasculitic pathologies have been described to occur in relation to HIV-associated brain vasculitis: granulomatous angiitis, eosinophilic vasculitis, and nonspecific small-vessel angiitis (which necessitates the performance of a brain biopsy).2
FIGURE 2
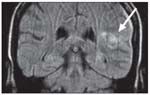
The obstruction seen in
Figure 1
might account for the cortical and subcortical edema
The patient was advised to undergo a brain biopsy, but she adamantly refused. Antiepileptic therapy was started for symptomatic management. The seizures were controlled, with no recurrence or neurological sequellae.
A medical literature search suggested the use of HAART for HIV-associated neurological disorders, including vasculitis.3,4 Corticosteroids also could be considered for patients with refractory HIV-associated vasculitis,5,6 although the bulk of evidence favors their use for non–HIV-related primary CNS vasculitis.7
Conclusions
Primary CNS vasculitis in HIV, a rare disease entity that it is poorly characterized, has been seen less frequently since the introduction of HAART for HIV management. MRA findings often suggest the diagnosis for a susceptible patient. The diagnosis of HIV-associated CNS vasculitis is a diagnosis of exclusion that requires ruling out other infectious and autoimmune causes. Brain biopsy can establish the diagnosis, although it is not always performed. There is very little published evidence to guide the diagnosis and appropriate treatment.
References:
References
1. Mandell BF, Calabrese LH. Infections and systemic vasculitis. Curr Opin Rheumatol. 1998;10:51-57.
2. Saravanan M, Turnbull IW. Brain: non-infective and non-neoplastic manifestations of HIV. Br J Radiol. 2009;82:956-965.
3. Gupta S, Shah DM, Shah I. Neurological disorders in HIV-infected children in India. Ann Trop Paediatr. 2009;29:177-181.
4. Maniar AJ, Maniar JK, Kamath R, et al. Primary HIV-1 infection-a “window of opportunity” for healthcare providers. J Assoc Physicians India. 2008;56:628-632.
5. van Boekel V, Assuf S, Godoy JM, et al. Isolated vasculitis of the central nervous system and involvement of the 8th cranial nerve: rare manifestations of acquired immunodeficiency syndrome [in Portuguese]. Arq Neuropsiquiatr. 1992;50:104-109.
6. Melica G, Brugieres P, Lascaux AS, et al. Primary vasculitis of the central nervous system in patients infected with HIV-1 in the HAART era. J Med Virol. 2009;81:578-581.
7. HAli RA, Singhal AB, Benseler S, et al. Primary angiitis of the CNS. Lancet Neurol. 2011;10:561-572.

Real-World Study Confirms Similar Efficacy of Guselkumab and IL-17i for PsA



