Article
Cognitive Performance Significantly Lower in Patients With SLE
Author(s):
The cross-sectional analysis determined cognitive performance of patients with systemic lupus erythematosus was significantly lower when compared with controls in both motor speed and psychomotor speed domains.
Motor speed and psychomotor speed were significantly lower in patients with systemic lupus erythematosus (SLE), both with neuropsychiatric manifestations (NPSLE) and without (non-NPSLE), when compared with healthy controls, according to a study published in BMC Rheumatology.1
“Among the many symptoms that SLE patients can experience, problems with cognitive functioning are frequently reported,” investigators stated. “While a number of studies have addressed the cognitive functioning of SLE patients, research on the longitudinal course of cognitive impairment in this population and potential fluctuations over time is still limited.”
In this longitudinal, prospective study, a total of 91 right-handed, female patients with NPSLE (n = 33), non-NPSLE (n = 29), and healthy controls (HC) (n = 29) participated in standardized neurocognitive testing, including cognitive ability tests involving memory, function, and attention. Right-handed patients were chosen to reduce the risk of hemispheric differences that may impact the Magnetic Resonance Imaging (MRI) part of the analysis. Eligible patients were recruited from a pre-existing SLE cohort at the Clinic of Rheumatology in Lund, Sweden, had a verified diagnosis of SLE, and fulfilled 4 or more American College of Rheumatology (ACR) classification criteria for SLE. Both neurological and clinical examinations were performed.
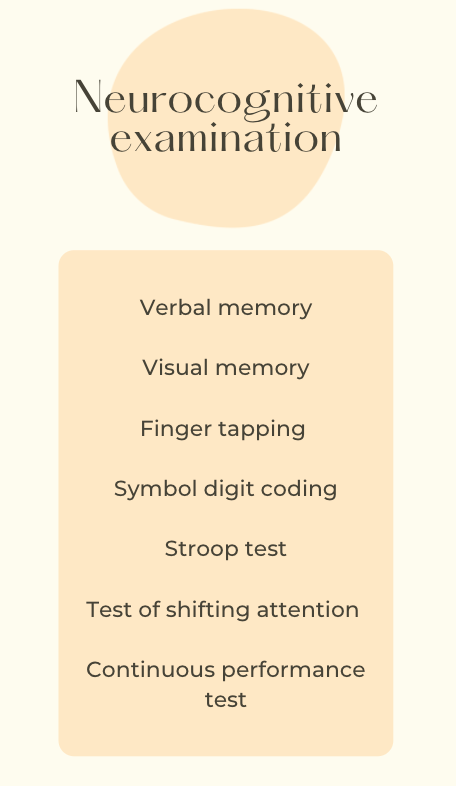
Longitudinal tracking was executed in 30 patients with NPSLE, 22 with non-NPSLE, and 13 HC, with cognitive evaluations focusing on domains such as simple attention, complex attention, motor speed, and psychomotor speed. Analyses of Variance (ANOVA) was utilized to analyze cognitive performance differences cross-sectionally across cohorts. Linear mixed effects models compared differences over time.
Overall, cognitive performance was normal to high in 97% of HC, 76% of patients with NPSLE, and 69% of patients with non-NPSLE. The cross-sectional analysis determined cognitive performance of both SLE groups was significantly lower when compared with HC in both motor speed and psychomotor speed. Further, patients in the NPSLE cohort performed significantly worse in the complex attention domain when compared with HC.
Both NPSLE and non-NPSLE cohorts performed similarly in all domains. Slight positive correlations were observed between disease duration and psychomotor speed, motor speed, and reaction time.
Several limitations should be addressed, including the lack of longitudinal effects due to varying test-retest intervals and the small sample size. It is also difficult to determine a direct correlation between SLE and neuropsychiatric problems in mild cases. Investigators did not take education into account and scheduling follow-ups during daytime work hours may have excluded some of the original participants from follow-up examinations.
“Some deviations in terms of the specific cognitive domains that are primarily affected in NPSLE and non-NPSLE patients notwithstanding, the findings of this study are overall in line with existent literature, which found cognitive deficits to be a reliable manifestation in the population of SLE patients as a whole,” investigators concluded. “In the future, further longitudinal examinations of the cognitive abilities of SLE patients will be essential to help the field gain a more refined understanding of how cognitive dysfunction develops in these patients over time.”
Reference:
Langensee L, Mårtensson J, Jönsen A, et al. Cognitive performance in systemic lupus erythematosus patients: a cross-sectional and longitudinal study. BMC Rheumatol. 2022;6(1):22. Published 2022 Apr 20. doi:10.1186/s41927-022-00253-3




