News
Article
Dermatology Skills for Internal Medicine Physicians with Roy Colven, MD
Author(s):
This presentation at ACP Internal Medicine 2024 covered key skills Colven believes internists should know for identification of dermatologic conditions.
In his American College of Physicians (ACP) Internal Medicine Meeting presentation ‘Dermatology for the Internal Medicine Physician: Honing Your Skills,’ Roy Colven, MD, professor at University of Washington, discussed approaches he believes internists should take in the diagnosis, management, and referral of patients with skin disease.
Colven covered many topics, discussing his experiences working in Cape Town as well as general rules he believes internal medicine physicians should be aware of if they encounter skin diseases. Some of the questions he sought to answer included common rashes to be able to recognize and manage, lesions to never miss, conditions which require referral and/or biopsies, and topical treatments to utilize.

Initially, he described the necessity of performing thorough skin examinations with good lighting and magnification as needed, noting that clinicians should pay attention to skin color variations impacting visibility of lesions.
“In the natural light is best and I would invest in a small flashlight,” Colven explained. “A hand lens is best and 4X is all you need.”
Colven humorously noted the common view among internists that a dermatoscope is needed, but he cautioned internists against buying a dermatoscope due to the lack of necessity. He also noted the value of the Epic Haiku system and of digital photography, as opposed to simple written descriptions of symptoms.
As far as diagnostics, Colven explained that internists should aspire to learn the following skills in their practice:
- Implementing an ‘exam-first’ approach to assessing skin conditions;
- Collecting specimens for KOH preparation;
- Interpreting KOH preparation confidently
- Describing lesions on skin accurately (e.g., papules, pustules, scales, etc.);
- Recognizing the different ways inflamed skin appears depending on skin color differences;
- Using a punch or shave biopsy on the body or the limbs, and even patients’ faces;
- Utilizing the ABCDEs and looking for “ugly ducklings” of skin conditions when assessing patients with lots of pigmented lesions.
“One condition that may give you a little bit of a break with respect to how it looks in different skin tones is psoriasis,” Colven said. “Well-demarcated, micaceous scale, salmon-colored plaques…The contrast is greater here but here it's not terribly subtle. I think you can find that it gets a little trickier when we look at more serious conditions.”
Colven showed several images of different conditions and highlighted the fact that those with darker skin tones versus lighter skin tones showed differing signs of disease, depending on the condition. He added that while many conditions are more visible on lighter-skinned patients, darker-skinned patients often show signs of vitiligo more clearly.
Later in his presentation, Colven discussed the use of various types of therapeutics and skills he hopes internists will implement or continue implementing.
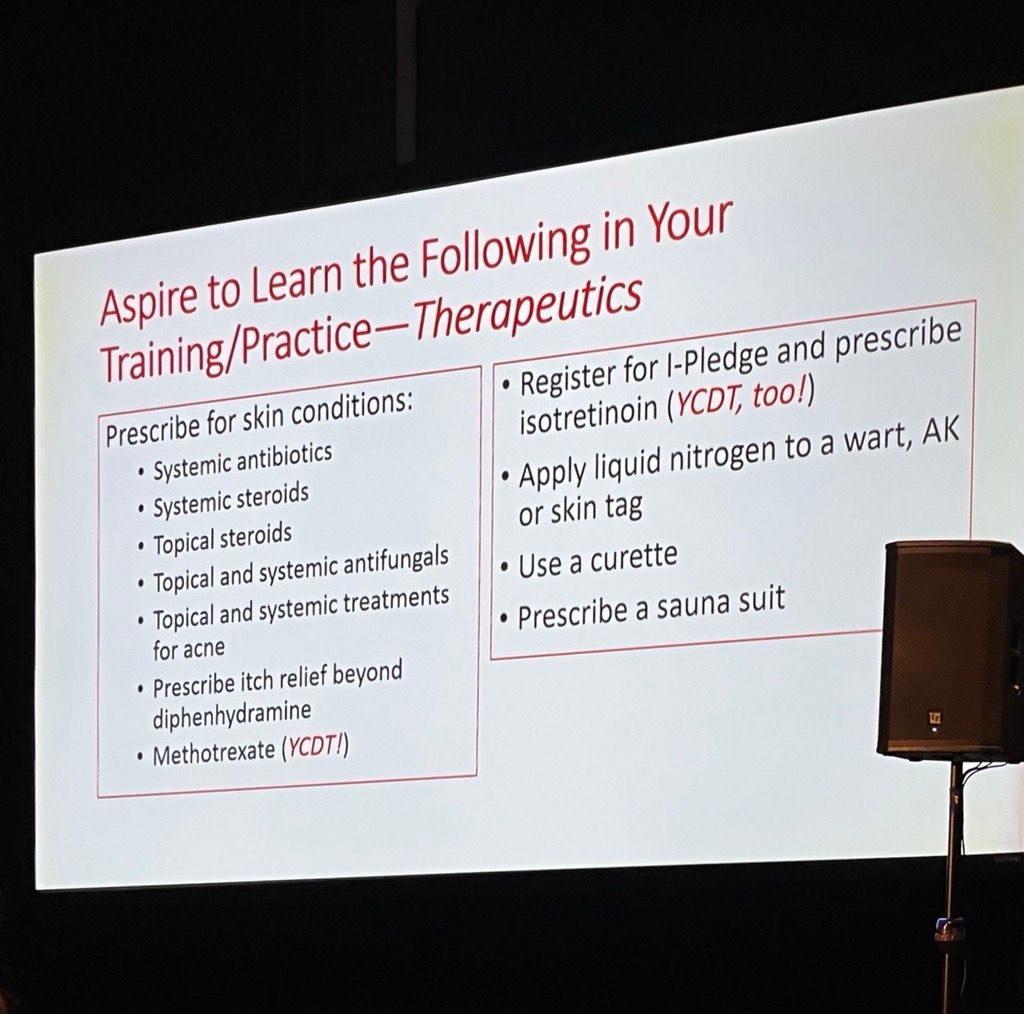
“Here's what I'd like to see you aspiring to learn in your practice,” Colven said. “So some of these things you already do, or some of these things you do for other reasons, but you can apply them to a dermatological condition.”
For skin condition prescriptions, Colven noted that internal medicine physicians should use the following more often in their practices: Systemic steroids, systemic antibiotics, topical and systemic antifungals, topical steroids, topical and systemic acne treatments, itch relief treatments beyond diphenhydramine, and methotrexate. Methotrexate specifically was praised by Colven, as an older treatment option that still works really well.
Additionally, Colven explained that internists should register for I-Pledge and prescribe isotretinoin for patients with acne. He further suggested that internists should utilize a curette for treating corns (the best of which he states are disposable), prescribe a sauna suit for rashes after a topical steroid to humidify the skin, and apply liquid nitrogen to warts, actinic keratosis, or skin tags.
“If you're getting liquid nitrogen sent to your clinical practice, you might as well administer (liquid nitrogen) with something that works well,” Colven stated, adding that the ‘cup and Q-tip’ mode does not work well. Colven recommends the version that costs $639 for clinical practices.
Overall, Colven’s presentation at the ACP Internal Medicine Meeting provided several potentially-invaluable insights for internal medicine physicians looking to expand their knowledge of dermatologic disease diagnosis and management.
For further conference coverage, view our conference page here.





