Article
Early Achievement of Minimal Disease Activity Linked to Better Outcomes in Psoriatic Arthritis
Author(s):
Patients with psoriatic arthritis who achieve minimal disease activity during the first year of diagnosis are shown to experience better health-related quality of life, improved mental wellbeing, and reduced fatigue.
In patients with psoriatic arthritis (PsA), failure to achieve minimal disease activity (MDA) by 1 year was linked to worse patient-reported outcomes (PROs), which persisted over time, according to a study published in Rheumatic and Musculoskeletal Diseases.1
“Previous studies have shown that patients with PsA who achieve MDA are less fatigued and have better health-related quality of life (HRQoL), mental well-being, and worker productivity than patients who do not reach MDA,” investigators stated. “The importance of achieving MDA within the first year for improved HRQoL at 12 months has also been demonstrated. However, there are hardly any studies with long-term data to support this.”
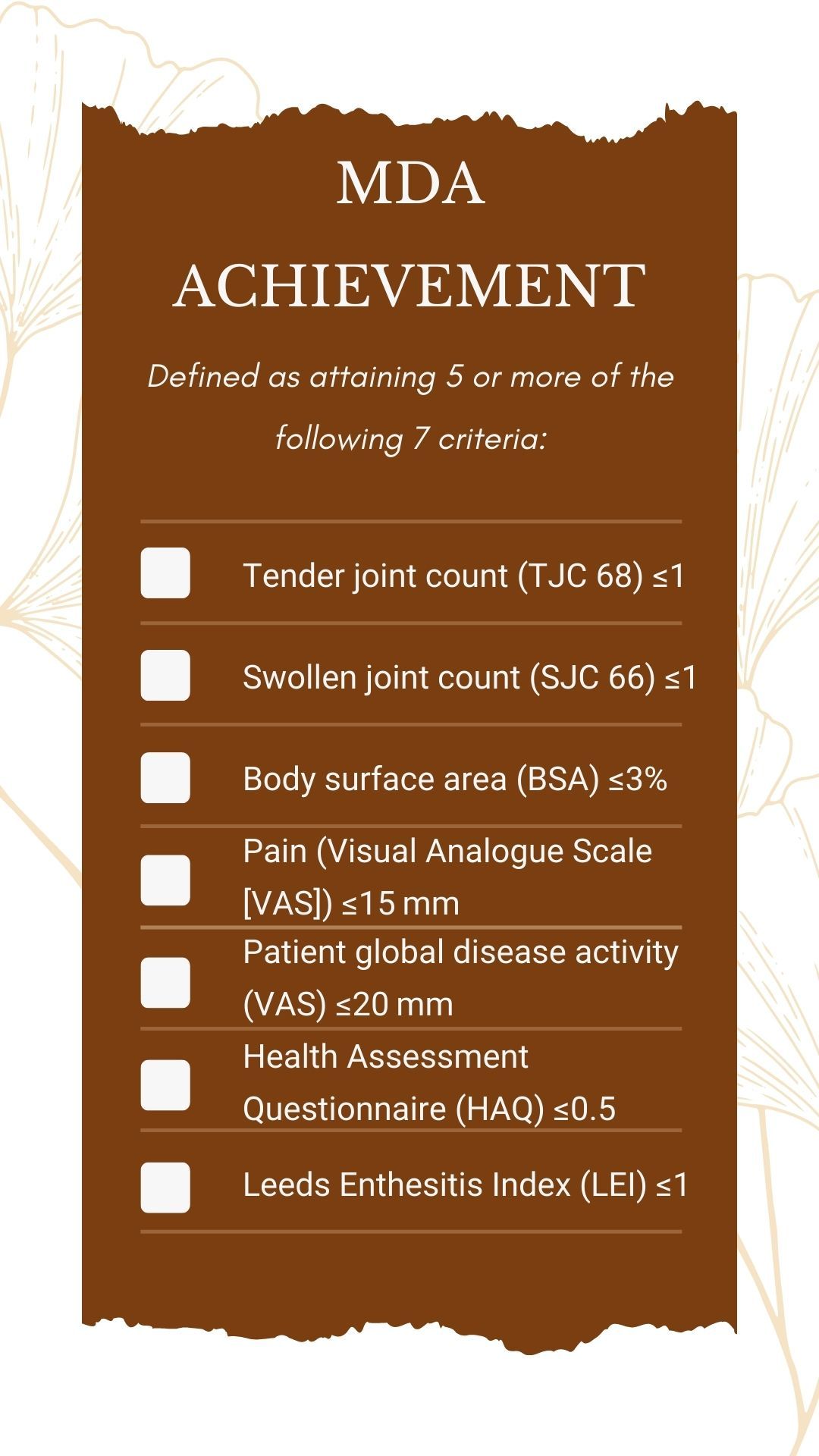
The impact of MDA was evaluated using data from newly diagnosed patients with PsA who were disease-modifying antirheumatic drug (DMARD) naïve and had oligoarthritis (2-5 joints) or polyarthritis (more than 5 joints) at baseline. Patients were chosen from the Dutch southwest Early PsA cohoRt (DEPAR). MDA was defined as achievement of 5 or more of the 7 criteria assessing both clinical aspects and PROs. Follow-ups were performed every 3 months during the first year, every 6 months in year 2, and once a year during year 3.
Patients were classified into 3 groups: those who achieved MDA at 9 and 12 months after PsA diagnosis (sustained MDA), patients who achieved MDA within the first year but did not sustain it at both 9 and 12 months (non-sustained MDA), and those who did not achieve MDA by 1 year (no MDA). PROs were compared between the cohorts from the first year to year 3.
Of the 240 patients included in the study, 43% (n = 104) had sustained MDA, 25% (n = 60) were placed in the non-sustained MDA group, and 32% (n = 76) were not able to achieve MDA. The mean age at baseline was 52.8 years, 51% (n = 122) were male, and the median symptom duration was 9.4 months.
Compared with the sustained MDA group, patients with no MDA had significantly lower PROs during follow-up appointments when compared with both the sustained MDA group and the non-sustained MDA group. The health status, determined by the European Quality of life 5-Dimensions 5-Levels (EQ-5D-5L), was 0.23 units lower in the no MDA group (95% CI −0.28 to −0.18), and functional impairment, evaluated using the Health Assessment Questionnaire-Disability Index (HAQ-DI) was 0.81 units higher (95% CI 0.70 to 0.92).
Visual Analogue Scale (VAS) scores reported that pain was 35.38 mm higher in patients who did not attain MDA (95% CI 30.57 to 40.18) and 15.80 mm higher in the non-sustained MDA group (95% CI 10.71 to 20.89) when compared with those who were able to sustain MDA. Fatigue, as examined using the Bristol Rheumatoid Arthritis Fatigue-Multidimensional Questionnaire, was also 17.88 units higher (95% CI 14.60 to 21.16) in the non-MDA cohort and 7.87 units (95% CI 4.40 to 11.33) higher in the non-sustained MDA cohort when compared with the sustained MDA cohort.
The Hospital Anxiety and Depression Scale indicated that levels of both anxiety (3.26-unit increase [95% CI 2.25 to 4.27]) and depression (4.04-unit increase [95% CI 3.10 to 4.99]) were statistically higher in patients who did not achieve MDA compared with the other groups.
Results of the study are more generalizable when compared with other trials because the DEPAR includes patients with PsA who are receiving usual care. Additionally, data collection was performed in a standardized manner by research nurses, thus ensuring reliability. However, many of the PROs across different International Consortium for Health Outcome Measurement (ICHOM) domains were assessed, leading to multiple testing. To counteract this, investigators used a Bonferroni correction, which showed consistent differences between the 3 groups. Finally, an underestimation of results may have occurred due to selective dropout, with reasons for discontinuation including inactive disease or dissatisfaction with treatment.
“To reduce the burden of PsA, early intensive treatment focusing on all facets of the disease, including associated comorbidities, is necessary,” investigators stressed. “In patients who do not achieve MDA despite early escalation of therapy, we need to look beyond biologic DMARDs (bDMARDs) and be aware of comorbidities and other factors that affect their ability to achieve MDA.”
Reference:
Snoeck Henkemans SVJ, de Jong PHP, Luime JJ, et al. Importance of quick attainment of minimal disease activity for a positive impact on lives of patients with psoriatic arthritis. RMD Open. 2022;8(2):e002706. doi:10.1136/rmdopen-2022-002706





