Evaluating hip pathology in trochanteric pain syndrome
Patients may have greater trochanteric pain syndrome foryears without knowing a defining cause or seeing pain improvement.Pathology within and around the hip joint falls into one of severalcategories, including acute pain with trauma, overuse and repetitivemotion activities, and diseases and degenerative conditions. Pain isdescribed as deep, occasionally sharp aching and stiffness. A uniqueset of factors contribute to the stability and function of the joint. Thedifferential diagnosis for hip pathology includes many entities; consideringreferred pain patterns is important to reduce inappropriatetesting.A compartmental approach to testing for hip pathology helpsorganize causes. Plain radiographs are an important first step inimaging; MRI may help delineate the sources of pain. (J MusculoskelMed. 2008;25:428-436)
ABSTRACT: Patients may have greater trochanteric pain syndrome for years without knowing a defining cause or seeing pain improvement. Pathology within and around the hip joint falls into one of several categories, including acute pain with trauma, overuse and repetitive motion activities, and diseases and degenerative conditions. Pain is described as deep, occasionally sharp aching and stiffness. A unique set of factors contribute to the stability and function of the joint. The differential diagnosis for hip pathology includes many entities; considering referred pain patterns is important to reduce inappropriate testing. A compartmental approach to testing for hip pathology helps organize causes. Plain radiographs are an important first step in imaging; MRI may help delineate the sources of pain. (J Musculoskel Med. 2008;25:428-436)
Greater trochanteric pain syndrome (GTPS)-tenderness without inflammation along the side of the hip-often is misdiagnosed because it shares pain patterns with other musculoskeletal conditions. Patients may have the condition for years and may have presented to several clinicians, undergone extensive diagnostic testing, and received several therapies-without seeing a defining cause or improvement of their pain. Undiagnosed hip conditions such as this may result in considerable pain for a frustrated patient who often is labeled a malingerer.
Patient evaluation for GTPS begins with an accurate history and physical examination. Serial diagnostic and therapeutic injections may play an important role in management. Radiological studies, including MR arthrography, often are indicated.
In this 2-part article, we describe the diagnosis and management of hip pathology in GTPS. This first part focuses on patient evaluation and the differential diagnosis. In the second part, to appear in a later issue of this journal, we will discuss approaches to treatment.
MECHANISM
Pathology within and around the hip joint falls into one of several categories. Acute onset of pain most often is the result of trauma. Acute pain and injury have been observed after a twisting motion. Pathology also may result from overuse and repetitive motion activities. Another category is diseases and degenerative conditions that may result in biomechanical alteration of the structural components of the joint.
CLINICAL PRESENTATION
Pain, a common presentation, is described as deep, occasionally sharp aching and stiffness in the hip. Pain may be localized to the proximal, lateral aspect of the thigh and pelvic rim. Patients often describe the location of pain by cupping their hand over the greater trochanteric region.
The pain may radiate into the groin and down the lateral aspect of the thigh.1,2 It may be confused with pain referred from the lumbosacral spine or sciatic nerve.1,3 A catching or locking of the joint may be noted. The pain may be referred to the level of the knee but rarely is found to be more distal.4 Patients also may note numbness and symptoms in the upper thigh that do not follow a typical lumbar dermatome segment.4
Pain may worsen in the trochanteric and gluteal region with almost any movement and with lying on the affected side. Rising from a seated position exacerbates the condition; patients may require a cane for ambulation. They may have an altered gait because of weakness resulting from the underlying pathology or from guarding. The pain often improves with rest and gradually increases as the day progresses. Compensatory spasm in the surrounding musculature may further mask the hip pathology with overlapping pain patterns (eg, sciatica resulting from piriformis syndrome or iliotibial band syndrome).
A history of an associated injury or fall may provide insight into the nature of the injury. Past history of congenital or childhood abnormalities may be a contributing factor because of altered biomechanics.
ANATOMY AND BIOMECHANICS
The hip traditionally has been classified as a ball-and-socket joint (Figure). A unique set of factors contribute to the stability and function of the acetabulofemoral joint. Factors that affect the biomechanical integrity of the joint include muscular attachments, cartilaginous and ligamentous structures, and the joints above and below the central hub. Alteration of the relationship between the femur and acetabular fossa may result in undue wear and eventual disruption of these cartilaginous surfaces within the joint and, therefore, pain.
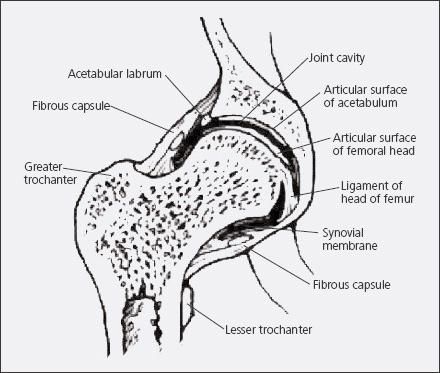
Figure –
Factors that affect the biomechanical integrity of the hip, or acetabulo-
femoral, joint-traditionally classified as a ball-and-socket joint-include muscular attachments, cartilaginous and ligamentous structures, and the joints above and below the central hub. Alteration of the relationship between the femur and acetabular fossa may result in undue wear and eventual disruption of these cartilaginous surfaces and, therefore, pain.
Medially, superiorly, and posteriorly, the hip is loaded via the sacroiliac joint, which transmits weight from the axial spine. Medially, anteriorly, and inferiorly, the pubic symphysis functions as a point of stabilization, doing so for both hips. These points of attachment may affect the angle and rotation of the acetabular fossa. Inferiorly, the stability and alignment of the lower extremity kinetic chain may affect the seating of the femoral head into the acetabular fossa.
A fibrous capsule encases the acetabulofemoral joint, forming the central joint cavity. A synovial layer that secretes the viscous synovial fluid lines this capsule. The ligamentum teres anchors the head of the femur to the acetabulum inferiorly and anteriorly. The acetabular fossa and the femoral head are covered with hyaline cartilage. A meniscus-like fibrocartilaginous labrum rims the fossa, allowing for load redistribution as the joint experiences weight transfer.
Muscular support of the hip is best described by function. Flexion and extension are the primary movements of the joint. The iliopsoas serves as the primary flexor; the rectus femoris and the other muscles passing anterior to the pelvic rim are secondary flexors. Extension is accomplished primarily by the gluteus maximus in collaboration with the medial and lateral hamstring complexes. Flexion is to 135°, and extension reaches 15°. These muscle groups act as restraints to the opposing contracting group.
Joint rotation is not as full as that seen in the shoulder but still is a crucial function. The rotator cuff of the hip consists of 2 groups of hip muscles, the abductors (30° to 50°) and external rotators (40° to 60°). The gluteus medius acts as the primary abductor, and secondary contribution comes from the gluteus minimus. Insertion for both is into the anterior, lateral aspect of the greater trochanter in the peripheral compartment, pulling toward their origin at the posterior rim of the iliac crest. External rotators that attach at the posterolateral aspect of the greater trochanter include the piriformis, superior and inferior gemellus, obturator internus and externus, and quadratus femoris.
Pelvic stabilization is maintained by the lateral and medial muscles of the hip. Medially, this is accomplished by the 3 adductors (longus, brevis, and magnus), along with the gracilis and the pectineus to 30°. Internal rotation of the hip (30° to 40°) is a weak movement accomplished by muscles passing anterior to the joint. These include the adductors and iliopsoas, as well as the anterior fibers of the gluteus medius and minimus. The resting position of the hip occurs at 30° of flexion, 30° of abduction, and slight external rotation.
The trochanteric region contains 3 bursae lying beneath the iliotibial band and along the greater trochanter. The largest bursa is roughly 2 to 4 cm in width and 4 to 6 cm in length. It lies between the gluteus maximus tendon; the converging fibers of the tensor fascia lata, where the iliotibial band (ITB) is formed; and the underlying gluteus medius tendon.4,5 The middle bursa lies between the tendons of the gluteus medius and gluteus minimus and the lateral superior border of the greater trochanter. The smallest bursa lies between the gluteus minimus and greater trochanter.4,6 A small bursa lying below the iliopsoas tendon forms its own compartment. These bursae facilitate gliding between adjacent structures.
Innervation of the region surrounding the greater trochanter is supplied by branches of the iliohypogastric nerve, the obturator, and the femoral and sciatic nerves. The subcostal nerve or the second, third, or fourth lumbar plexus also is involved.1
DIFFERENTIAL DIAGNOSIS
The differential diagnosis for hip pathology includes many entities; multiple conditions often contribute to the patient's pain. A diagnosis of peripheral or causation etiology often is made, and the underlying primary lesion remains undiscovered. Therefore, considering these referred pain patterns in the differential diagnosis is important to reduce inappropriate testing (Table 1).2

PHYSICAL EXAMINATION
Observation
On entering the room, the patient may exhibit a Trendelenburg gait and use a cane or walker. He or she may take a sitting or standing position to relax the abductors and alleviate the pain. Almost any movement may worsen pain in the trochanteric and gluteal region. Rising from a chair may induce pain; weakness in the affected limb may be observed by noting use of the ipsilateral upper extremity to push up from sitting.
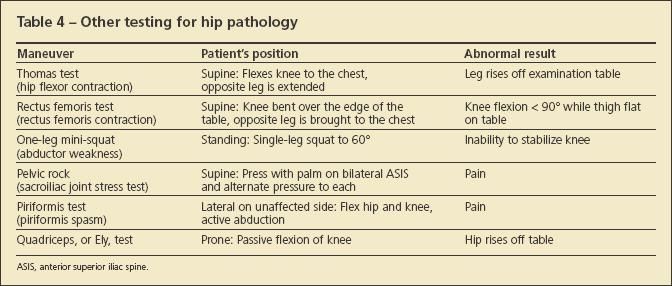
Once the patient is standing, the Trendelenburg test, which examines the ability of the hip abductors to stabilize the pelvis on the femur, may be used for simple yet effective evaluation. The patient stands first on the unaffected side and then on the affected side. A normal test result is indicated when the pelvis rises on the opposite side or the pelvis remains level. An abnormal result is seen when the pelvis on the opposite side drops, indicating a weak or painful gluteus medius. A failed test also should raise suspicion that these structures may be disrupted.
If the Trendelenburg test result is normal, a one-leg mini-squat is used for assessment. Inability to maintain control of the knee because of abductor and core instability is evaluated.
Palpation
The patient is directed to lie on the examination table, at first on his unaffected side. The knee and hip of the affected extremity are held in moderate flexion. The examiner then begins palpation from inferior to superior while assessing for pain. An abnormal test result is elicited by having the patient report pain on palpation inferiorly and at the level of the firm bony trochanter.7
Pain on direct palpation of the trochanter results in a positive "jump" sign (the patient "jumps" because of the pain).6,8 This result is indicative of lateral compartment pathology. Pain on palpation at the anterior, lateral aspect of the greater trochanter points toward a potential disruption of the gluteus medius or minimus from its insertion. Anterior tenderness at the iliopectinate line may be the result of iliopsoas bursitis. The patient may have complaints of a snapping sound with this tenderness. Pain or tenderness over the sacroiliac or piriformis may be the result of compensatory problems and represent their own contributing pathology, making the underlying primary injury difficult to identify.
Range of motion
This should be documented in all examinations. Because range of motion and clinical tests involving hip movement may elicit pain, however, their use may not help the examiner find the source of pain.
Maneuvers
A compartmental approach is presented to organize causes of hip pathology. Structuring the examination by beginning centrally and working out from the femoroacetabular joint helps identify the contributing factors in the patient's complaint.
The patient is asked to lie in the supine position with the affected leg on the side of the examiner. The log roll test is an initial nonspecific examination method used to confirm that the pain is attributed to the hip joint. An abnormal finding is indicated if pain is noted while the leg is held in extension with the foot internally and externally rotated. A normal evaluation result does not preclude hip pathology. Pain with log rolling may be nonspecific or, more ominously, could represent hip fracture; imaging studies are indicated.
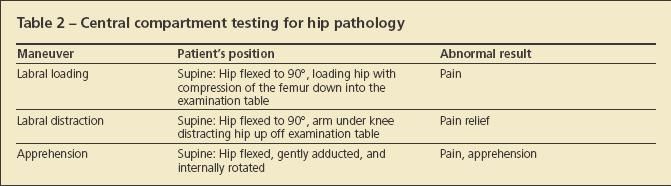
• Central compartment testing. Evaluation of the central compartment is conducted with the integrity of the central structures in mind. Labral loading is performed with the patient supine and the affected leg flexed (Table 2). The examiner places the knee in his or her armpit, compressing the femoral head into the acetabulum. If pain is elicited, the test result is considered abnormal, pointing toward labral or cartilaginous pathology. Labral distraction is the reverse, lifting the hip off the examination table at the knee. Pain relief is considered confirmatory.
When conducted properly, apprehension testing evaluates patients for incongruity of the labral rim; pain or apprehension indicates an abnormal result. The hip is again flexed adducted and internally rotated. The test result also may be abnormal with peripheral compartment impingement, such as "Cam" or "pincer" impingement.
• Peripheral and lateral compartment testing. To date there is no physical examination test to define peripheral compartment pathology. The lateral, or trochanteric, compartment often produces an aching pain over the lateral hip that is exacerbated by activity (eg, prolonged standing, lying on the ipsilateral side, stair climbing, or running). Although the classic symptom is lateral hip pain, pain may radiate to the groin or, in about one-third of patients, into the lateral thigh. Pain resulting from a straight-leg raise as the ITB slides past the trochanter may be referred from the lateral compartment (Table 3).
The Ober test is another assessment for ITB contracture. The patient lies on his side with the hips and knees flexed. The upper leg is passively abducted and extended. The limb is then lowered to the table. If there is contracture, the leg does not fall to the table. The hip is stabilized to prohibit the patient from rolling backward and to allow the ITB to slip over the greater trochanter.
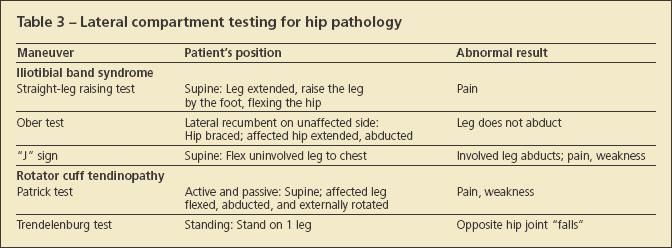
The "J" sign may be performed with the patient supine by flexing the uninvolved leg. If the painful hip abducts, a restricted ITB is confirmed.
On examination, pain is reproduced with external rotation and abduction and by resisted abduction. An abnormal Patrick test result and hip weakness may represent gluteus medius tendinopathy, which is distinguished by tenderness on palpation superior to the greater trochanter. Tendinopathy of the gluteus medius and minimus may lead to progressive changes at the insertion on the trochanter resulting from tendinitis or tendinosis of the muscles inserting into the greater trochanter as well as the ITB as it glides along the greater trochanter. Inflammation in the tendons is thought to arise from microtrauma in the tendons resulting from overuse or injury.4,9
Rupture of the tendons inserting into the greater trochanter may be the long-term result of hip tendinitis. The description of these tears resulting in a "bald trochanter" has been aptly described as a rotator cuff tear of the hip.10,11
Patients often have pain for quite some time before presenting with complete rupture of the tendons of the trochanter. In addition to the expected pain from palpation, examination in these patients reveals an abnormal Trendelenburg gait and significant weakness or inability to complete a single repetition of the one-leg mini-squat test.5 Significant weakness on core muscle testing also may direct the clinician to the source of pain resulting from abductor muscle deficiency.5
• Iliopsoas compartment testing. Several tests may elicit an abnormal finding if the cause lies within the fourth and final compartment of the hip, the iliopsoas compartment. An abnormal result of the Patrick test, along with an abnormal test result of anterior or medial groin pain, may indicate iliopsoas spasm.
The psoas test is conducted with the hip flexed to 30º while the patient attempts to raise the knee against resistance. An abnormal result is pain, indicating psoas muscle pathology. Anterior hip or groin pain may result from iliopsoas or iliopectineal bursitis. The cause of pain is thought to be irritation of the iliopsoas tendon over the iliopectineal eminence. Placing the hip in flexion and external rotation relieves symptoms. Hip extension (stretching of the iliopsoas) exacerbates the symptoms. Use of additional testing is prudent to fully delineate pain generators throughout the hip joint (Table 4).
Imaging studies
Obtaining plain radiographs is an important first step in imaging for hip evaluation. The presence of mild degenerative changes does not exclude other hip pathology as the source of pain. Plain radiographs may demonstrate cystic changes seen around the greater trochanter, such as those that might be seen in rotator cuff pathology. Although the presence of trochanteric cysts does not indicate a tear of the gluteal musculature, the changes may direct the examiner to the tendinous insertions as one possible source of pain. Calcifying lesions, such as calcific tendinopathy, also may be present on x-ray films. Bony lesions (eg, fractures and space-occupying cystic lesions) often are seen on plain x-ray films.
MRI may help delineate the sources of pain in hip pathology. 9,12-14 This modality has documented tendinosis and tears of the gluteus medius; however, the true incidence is unknown because of selection bias in patients undergoing MRI.3
Edema seen in the bone and soft tissue may help delineate occult fractures, as well as gross tendinous ruptures. In addition, MRI may show fluid in the bursal regions and in adjacent soft tissue. Labral tears may be identified and are more evident when arthrography is used.
These pathologies are not always evident on MRI to even the most practiced radiologist. A normal result should not discourage referral when the history and physical examination results lead the clinician to a high index of suspicion for pathological disorders.
OTHER SOURCES OF PAIN
Low back pain often is associated with hip pathology.1-3,6,8,15 Pain elicited with a straight-leg raise as the ITB slides past the trochanter may be confused with trochanteric pain. Patients with GTPS may have pain with range of motion of the hips with resisted abduction and extremes of external rotation and abduction. Pain also may be referred to the groin and to the sacroiliac joint. Pain referred on range of motion of the hip may be confused clinically with hip osteoarthritis, because pain may radiate along the anterior groin and the posterior aspect of the hip.15
Pseudoradiculopathy of the lateral hip often is confused with trochanteric pathology. Patients with upper lateral thigh pain may have referred pain from the nociceptive fibers of the lumbar roots, facet joints, and paraspinous ligaments.3 Patients with lateral nerve root pain typically complain more of leg pain than of back pain, which may mislead the diagnosis. Pain typically does not extend below the knee in GTPS, but radicular pain often extends past this level.
The iliohypogastric nerve and subcostal nerves are the most common nerve entrapments in the hip region (Table 5). The most common site of entrapment of the iliohypogastric nerve is about 10 cm posterior to the anterosuperior iliac spine. At this level, the nerve crosses the iliac crest.3 The subcostal nerves may be trapped more posteriorly over the brim of the iliac crest.
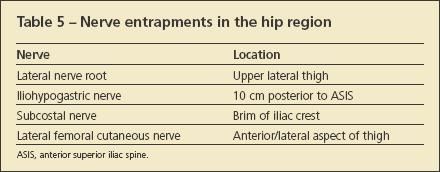
The lateral femoral cutaneous nerve also may refer pain to the lateral aspect of the thigh. In this case, the pain often is more anterior than lateral.3 Diagnostic injections of local anesthetic performed at the site of suspected nerve entrapment may be extremely beneficial in diagnosis. The diagnostic injection should result in almost immediate symptom improvement; if no improvement is noted, a secondary diagnosis must be considered.16
ATYPICAL CAUSES OF PAIN
Atypical sources of pain also may present as GTPS (Table 6). Diagnoses of osteonecrosis and femoral neck stress fractures have been reported when peritrochanteric pain was the presenting complaint.16,17 Diagnoses of mass-occupying lesions (eg, calcific tendinopathy, tuberculosis, giant cell carcinoma, and rheumatoid inflammation of the trochanteric bursa) have been made in patients with hip pain.15,18-26
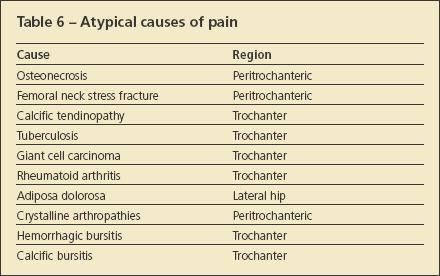
Adiposa dolorosa, a pain syndrome in which the subcutaneous fatty tissue at the lateral aspect of the hip generates pain evident on palpation, is very similar to GTPS.3 Patients typically are morbidly obese; pain is elicited on palpation of the fatty tissues rather than the trochanteric bursa.
Crystalline arthropathies also play a role in the development of symptomatic GTPS.21 Hemorrhagic bursitis after an acute fall and infectious bursitis also must be considered in the differential diagnosis. In addition, calcific bursitis is thought to occur as a result of dystrophic calcium deposition into the collagen matrix because of chronic inflammation.
References:
References
- 1. Shbeeb MI, Matteson EL. Trochanteric bursitis (greater trochanter pain syndrome). Mayo Clin Proc. 1996;71:565-569.
- 2. Karpinski MR, Piggott H. Greater trochanteric pain syndrome: a report of 15 cases. J Bone Joint Surg. 1985;67B:762-763.
- 3. Dickinson AM. Bilateral snapping hip. Am J Surg. 1929;6:97-101.
- 4. Spear IM, Lipscomb PR. Noninfectious trochanteric bursitis and peritendinitis. Surg Clin North Am. 1952;32:1217-1224.
- 5. Collée G, Dijkmans BA, Vandenbroucke JP, Cats A. Greater trochanteric pain syndrome (trochanteric bursitis) in low back pain. Scand J Rheumatol. 1991;20:262-266.
- 6. Tortolani PJ, Carbone JJ, Quartararo LG. Greater trochanteric pain syndrome in patients referred to orthopedic spine specialists. Spine J. 2002;2:251-254.
- 7. Clancy WG. Runners’ injuries, part two: evaluation and treatment of specific injuries. Am J Sports Med. 1980;8:287-289.
- 8. Larsson LG, Baum J. The syndromes of bursitis. Bull Rheum Dis. 1986;36:1-8.
- 9. Traycoff RB. “Pseudo-trochanteric bursitis”: the differential diagnosis of lateral hip pain. J Rheumatol. 1991;18:1810-1812.
- 10. Leonard MH. Trochanteric syndrome: calcareous and noncalcareous tendonitis and bursitis about the trochanter major. J Am Med Assoc. 1958;168:175-177.
- 11. Swezey RL. Pseudo-radiculopathy in subacute trochanteric bursitis of the subgluteus maximus bursa. Arch Phys Med Rehabil. 1976;57:387-390.
- 12. Tanaka H, Kido K, Wakisaka A, et al. Trochanteric bursitis in rheumatoid arthritis. J Rheumatol. 2002;29:1340-1341.
- 13. Kingzett-Taylor A, Tirman PF, Feller J, et al. Tendinosis and tears of gluteus medius and minimus muscles as a cause of hip pain: MR imaging findings. AJR. 1999;173:1123-1126.
- 14. LaBan MM, Weir SK, Taylor RS. “Bald trochanter” spontaneous rupture of the conjoined tendons of the gluteus medius and minimus presenting as a trochanteric bursitis. Am J Phys Med Rehabil. 2004;83:806-809.
- 15. Little H. Trochanteric bursitis: a common cause of pelvic girdle pain. Can Med Assoc J. 1979;120:456-458.
- 16. Willson JD, Dougherty CP, Ireland ML, Davis IM. Core stability and its relationship to lower extremity function and injury.
J Am Acad Orthop Surg. 2005;13:316-325.
- 17. Jones DL, Erhard RE. Diagnosis of trochanteric bursitis versus femoral neck stress fracture. Phys Ther. 1997;77:58-67.
- 18. Raman D, Haslock I. Trochanteric bursitis-a frequent cause of “hip” pain in rheumatoid arthritis. Ann Rheum Dis. 1982;41:602-603.
- 19. Mandell BF. Avascular necrosis of the femoral head presenting as trochanteric bursitis. Ann Rheum Dis. 1990;49:730-732.
- 20. Schein AJ, Lehmann O. Acute trochanteric bursitis with calcification. Surgery. 1941;9:771-779.
- 21. Crevenna R, Kéilani M, Wiesinger G, et al. Calcific trochanteric bursitis: resolution of calcifications and clinical remission with non-invasive treatment: a case report. Wien Klin Wochenschr. 2002;114:345-348.
- 22. Butcher JD, Salzman KL, Lillegard WA. Lower extremity bursitis [published correction appears in Am Fam Physician. 1996;54:468]. Am Fam Physician. 1996;53:2317-2324.
- 23. Ihara K, Toyoda K, Ofuji A, Kawai S. Tuberculous bursitis of the greater trochanter.J Orthop Sci. 1998;3:120-124.
- 24. King AD, Griffith J, Rushton A, Metreweli C. Tuberculosis of the greater trochanter and the trochanteric bursa. J Rheumatol. 1998;25:391-393.
- 25. Wakeshima Y, Ellen MI. Atypical hip pain origin in a young athletic woman: a case report of giant cell carcinoma. Arch Phys Med Rehabil. 2001;82:1472-1475.
- 26. Kamineni S, Southgate G. Trochanteric bursitis: an unusual operative finding. Orthopedics. 1999;22:1185-1186.





