Article
Gastric-Protective Aspirin Treatment Still Induces Peptic Ulcer
Author(s):
Even when it's administered in a low-dose form that resists gastric acid and prevents tablet dissolution in the stomach, aspirin therapy causes peptic ulcer and increases the risk of 30-day mortality resulting from gastrointestinal (GI) disorder progression.

Even when it’s administered in a low-dose form that resists gastric acid and prevents tablet dissolution in the stomach, aspirin therapy causes peptic ulcer and increases the risk of 30-day mortality resulting from gastrointestinal (GI) disorder progression, according to new research published in the Turkish Journal of Gastroenterology.
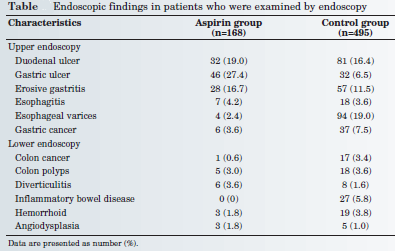
For their “Relationship between Continuous Use of Low-Dose Enteric-Coated Aspirin and Gastrointestinal Injuries in Patients with Gastrointestinal Hemorrhage” study, Mirhadi Mousavi, MD, from the Research Institute for Gastroenterology and Liver Diseases at the Shahid Beheshti University of Medical Sciences in the Islamic Republic of Iran and colleagues compared the upper and lower endoscopy findings of 168 patients taking 80 to 100 milligrams of enteric-coated aspirin per day to 495 non-aspirin users — all of whom had suffered GI hemorrhage.
Although the overall prevalence of duodenal ulcers was not statistically different between both patient groups, the researchers found peptic ulcer in 27.4 percent of patients in the aspirin group, compared to 6.5 percent of the non-aspirin group. Thus, the authors determined that “the use of low-dose enteric-coated aspirin could strongly predict gastric ulcers in patients examined by endoscopy.” (Table)

The endoscopies also detected greater H. pylori infection among the aspirin users, which was linked to peptic ulcer disease incidence as the authors wrote that “the overall prevalence of peptic ulcer disease in those with confirmed H. pylori infection was significantly higher than in the others (54.5 percent versus 10.4 percent).”
In terms of a patient’s risk of dying within 30 days after his or her first episode of GI bleeding, the authors found that aspirin use had a “main triggering effect on short-term mortality following gastrointestinal endoscopy,” since 10.1 percent of the patients treated with low-dose aspirin had early post-procedure mortality, compared to 5.9 percent of non-users.
Taking all of those findings into account, the researchers concluded that “low-dose enteric-coated aspirin causes significant gastric endoscopic lesions and even predicts short-term mortality due to progression of gastrointestinal disorders, (and) the adverse effect of low-dose enteric-coated aspirin on gastric mucosa is more severe in H. pylori infection.”





