Article
Genetic Investigation of Lymphotropism in Hepatitis C
Author(s):
Researchers address the controversial topic of B-cell infection by hepatitis C.
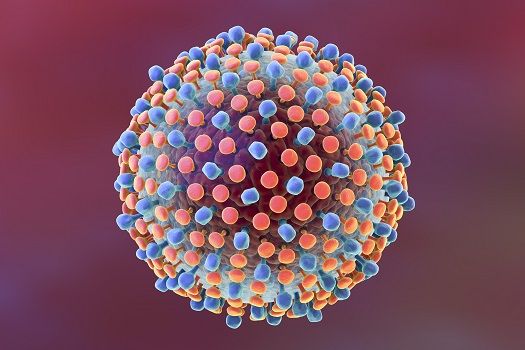
There is a genetic basis for lymphotropism in hepatitis C virus infection, found researchers from Keck School of Medicine at the University of Southern California.
Hepatitis C-associated lymphotropism is essentially when the pathogenesis of virus-related autoimmune and lymphoproliferative disorders overlap. Led by Chia-Lin Chen, PhD, of the Department of Molecular Microbiology and Immunology, the team conducted the study addressing the controversial topic of B-cell infection by hepatitis C. The topic remains unaccepted on a universal scale because there’s an insufficient amount of information on the topic.
The researchers began with the hypothesis that the sequence variation of the hepatitis C genome determined whether or not any given hepatitis C strain could infect B cells.
“We used genetic approaches to show that different hepatitis C strains vary in their relative lymphotropism or hepatotropism,” Chen and colleagues wrote in Nature Communications. Additionally, they examined how plasma miR-122 impacts hepatitis C pathogenesis and what kind of role exosome-mediated delivery of tropic factors plays in hepatitis C infection and replication.
First, the researchers compared the full-length ribonucleic acids (RNAs) from two strains of hepatitis C: SB-HCV, which they had previously isolated and knew could infect B cells, and JFH-1, which they say is “a well-established hepatotropic strain.” They used Huh7.5.1 cells, which are from a hepatocellular carcinoma cell line, and Raji cells, from a human B-lymphoid line, to compare how the two strains replicated.
There were two key findings. For one, “the SB-HCV strain, but not the JFH-1 strain, was able to replicate or was unstable RNA in Raji cells”. However, the converse was true in Huh7.5.1 cells, leading the researchers to say, the “Raji cells are more permissive for SB strain replication than Huh7.5.1 cells.”
Next, the researchers worked to identify the genome region or viral gene that is responsible for differential cellular tropism. For that investigation, the team continued to use the lymphotropic SB-HCV and the hepatotropic JFH-1 hepatitis C strains, but they constructed what they describe as “chimeric virus genomes.” The constructs were converted to RNA for transinfection. They say that the “results suggested that there are distinct hepatotropic and lymphotropic hepatitis C strains.”
Digging deeper, the researchers examined specific cellular structures and their importance to lymphotropism. Specifically, they examined the E1-E-2 proteins, the secondary structure of the SB 5’ UTR, how miR-122 levels affect replication, the co-receptors CLDN1 and OCLN, and the co-receptor B7.2.
The researchers conclude saying, “Hepatitis C tissue tropism is determined primarily by the properties of viral envelop proteins and the 5’-UTR, in addition to the ability of HCV to evade antiviral responses.” They add that this study and others like it open a new path for learning about extrahepatic hepatitis C infection.
The study, “Hepatitis C virus has a genetically determined lymphotropism through co-receptor B7.2,” was published in Nature Communications.
Related Coverage:
Interferon-Free 3D Treatment for Hepatitis C Works Fast
Multi-Genotype Hepatitis C Drug Application Lands in Front of the FDA
High Frequency of Tregs After Curing Hepatitis C Could Enhance Liver Cancer Risk





