Article
H. pylori Protein Presence Boosts Risk of Peptic Ulcer Disease
Author(s):
Though they conducted their analysis in China, four researchers have successfully demonstrated a link between babA2 gene and peptic ulcer disease (PUD) in Helicobacter pylori-infected populations within countries located on the Western Hemisphere.

Though they conducted their analysis in China, four researchers have successfully demonstrated a link between babA2 gene and peptic ulcer disease (PUD) in Helicobacter pylori-infected populations within countries located on the Western Hemisphere.
For their “Association of Helicobacter-pylori babA2 with Peptic Ulcer Disease and Gastric Cancer” study published in the July 14, 2013, edition of the World Journal of Gastroenterology, Mo-Ye Chen and three colleagues from the China Medical University reviewed 38 studies with a total of 4,556 patients from Asian or western populations in order to evaluate the relationship between babA2 — an “outer member protein of H. pylori, which plays a key role in facilitating bacterial colonization in the stomach” — and clinical outcomes.
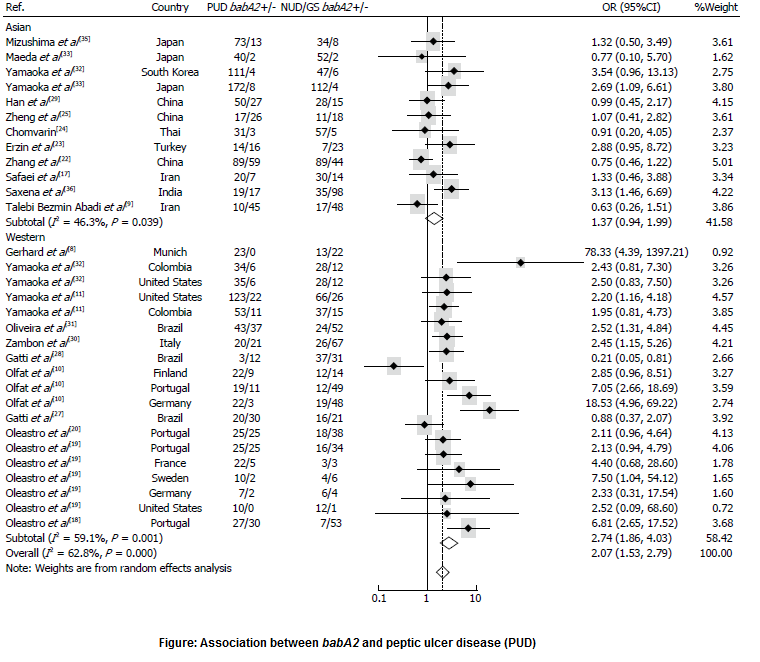
The researchers found babA2 in roughly 74 percent of the 1,859 patients with cases of PUD, compared to about 58 percent of the 1,909 control subjects with gastritis and/or non-ulcer disease (NUD). Interestingly, breaking down the data by geographic location showed that “in western countries, the presence of babA2 substantially increased PUD risk … while in Asian countries, the babA2 genotype was only borderline associated with PUD, (and) for duodenal ulcer (DU), the babA2 genotype significantly increased the risk of DU in western countries, but not in Asian countries.” (Figure) According to the authors, that “suggests a potential biomarker distinguishing PUD — especially DU — in western populations, and reveals a phylogenetic difference between Asian and western H. pylori strains.”
Though the researchers also compared the prevalence of babA2 gene in patients with gastric cancer and controls, they found no statistical association between the two, as the gene was present in approximately 71 percent of the 534 patients with cases of gastric cancer and about 61 percent of the 1,000 controls. The authors said the difference between the PUD and gastric cancer findings “may be partially due to the distinct etiologies of DU and GC development…(as) patients with DU rarely develop atrophic gastritis of the corpus, and therefore GC risk may decrease in such cases.”




