Article
Imaging for Dupuytren contracture
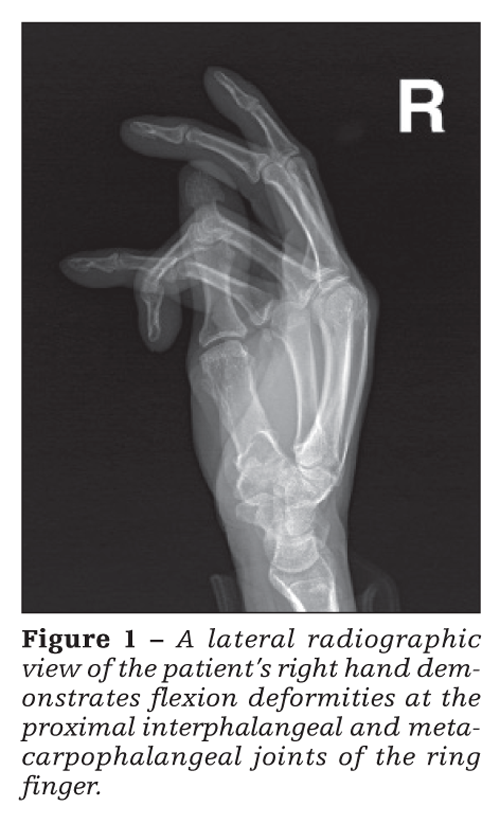
In Dupuytren contracture, hyperplasia of the palmar aponeurosis induces a contracture that typically involves the fourth and fifth digits of the hand. Radiographic findings consist of flexion deformity of the proximal interphalangeal joint of the ring finger, with mild subluxation.
ABSTRACT: In Dupuytren contracture, hyperplasia of the palmar aponeurosis induces a contracture that typically involves the fourth and fifth digits of the hand. Radiographic findings consist of flexion deformity of the proximal interphalangeal joint of the ring finger, with mild subluxation. MRI demonstrates low signal intensity compatible with fibrous tissue in the palmar soft tissue. The histology is characterized by fibroblast proliferation and collagen deposition. There are inherited and sporadic forms. The diagnosis is primarily clinical and is confirmed by pathology. Treatment may be conservative or surgical; nonoperative options include injection of collagenase clostridium histolyticum. Imaging is not routinely required. MRI is valuable in planning surgical treatment. (J Musculoskel Med. 2011;28:56-57)
In Dupuytren contracture, also called palmar fibromatosis, hyperplasia of the palmar aponeurosis induces a contracture that typically involves the fourth and fifth digits of the hand. Severe cases may show involvement of the third digit, but involvement of the first and second digits is exceedingly rare. In this article, we describe a clinical case report for a 58-year-old African American man with Dupuytren contracture who had a history of right ring finger deformity.
Clinical presentation
The patient, who was right-hand dominant, complained of long-standing flexion deformity of the right ring finger that was worsening. There was no family history of the deformity, and there were no plantar fibromas. The patient’s past medical history included asthma and hypertension. Physical examination of his right ring finger revealed fixed flexion deformity of the metacarpophalangeal (MCP) joint (70° of flexion) and of the proximal interphalangeal joint (PIP) joint (90° of flexion).
Radiographic and MRI findings in Dupuytren
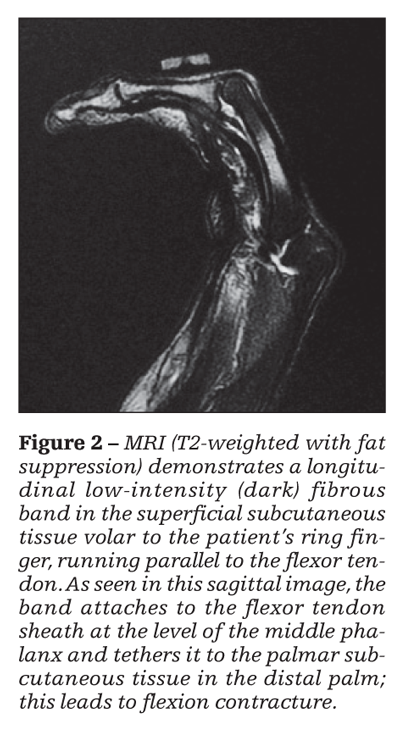
Radiographic findings in Dupuytren contracture consist of flexion deformities of the PIP and MCP joints of the ring finger, with mild subluxation at the PIP joint (Figure 1). MRI demonstrates low signal intensity compatible with fibrous tissue in the palmar soft tissue, with cord-like extensions along the fourth digit, that appears to be confluent with the flexor tendon and tethers the tendon at the PIP joint, consistent with Dupuytren contracture. This is shown in Figure 2 as the longitudinal dark band seen in the superficial subcutaneous tissue of the ring finger.
Pathology
The histology of Dupuytren contracture is characterized by fibroblast proliferation and collagen deposition, which lead to nodule and cord formation in the elements of the palmar fascia, with adherence to the skin, resulting in palmar contractures and flexion deformities. There is medial retraction of the neurovascular bundle.
Dupuytren contracture has both inherited and sporadic forms. When inherited, it is an autosomal dominant trait with variable penetrance. It is associated with other kinds of fibromatosis, such as plantar (10% of cases) and penile (Peyronie disease, 1% of cases). Sporadic or acquired forms have been described in relation to cirrhosis, chronic alcoholism, diabetes mellitus, seizures, and cigarette smoking.
Men are affected with Dupuytren contracture much more frequently than women. The condition is seen mostly in white persons, predominantly those of Celtic descent. Patients usually are past their fifth decade of life at presentation.
Diagnosis
The diagnosis of Dupuytren contracture is primarily clinical and is confirmed by pathology. Presentation in patients younger than 40 years is unusual, in which case an underlying condition, such as sarcoma, needs to be excluded with MRI.
Dupuytren contracture occurs bilaterally in 65% of patients; when unilateral, it occurs more frequently on the right side. The ring finger is most often affected, followed by the fifth and then the middle finger. The index finger and thumb usually are spared. The differential diagnosis includes stenosing tenosynovitis, trigger finger, a ganglion cyst, and a soft tissue mass (eg, sarcoma).
Treatment
Treatment for patients with Dupuytren contracture may be conservative or surgical. Nonoperative options include corticosteroid injection and injection of collagenase clostridium histolyticum, which was approved by the FDA in 2010 for use in treating patients with Dupuytren contracture. Surgical treatment consists of palmar dermofasciectomy and skin grafting.
Given the severity of his contracture, our patient opted for surgery. Under general anesthesia and with tourniquet hemostasis, he underwent surgical release of the contracture with dermofasciectomy and full-thickness skin graft reconstruction. The pathology of the excised volar skin and subcutaneous tissue revealed dense fibrosis and fibromatosis consistent with Dupuytren contracture. He received postoperative physical therapy in the form of digital manipulation and exercises in flexion and extension. On follow-up, he was able to achieve full extension and up to 90° of active flexion of the ring finger at the MCP and PIP joints.
Role of imaging
Imaging is not routinely required for Dupuytren contracture. However, MRI has a special role in defining palmar involvement. The higher the MRI signal intensity of the fibrous lesions (on T2-weighted images), the greater their cellularity. Increased cellularity correlates with an increased chance of recurrence.
Thus, MRI is valuable in planning surgical treatment. If the lesion is hypercellular, surgery may be delayed until an increase in collagen content is confirmed, as defined by hypocellularity on MRI, thus reducing the risk of
recurrence.




