Article
The Important, Evolving Role of Pharmacists in Helping Patients Quit Smoking
More than two-thirds of smokers want to quit, but lack proper resources. A prescribing professional could help make up that difference.
The health risks associated with tobacco smoking are well known among consumers and healthcare professionals. Despite this knowledge, the success rate for smoking cessation is low, in part because pharmacotherapy and counseling are under-utilized.
Data show that although 68% of smokers want to quit, only 6.8% utilize behavioral counseling, 29.0% utilize pharmacotherapy such as nicotine replacement therapy and/or non-nicotine prescription smoking cessation therapy (varenicline and bupropion SR), and only 4.7% used both.[1]
One of the factors that might play a key role in this underutilization of proven cessation resources is the barrier to accessing a medical professional who can prescribe smoking cessation medications at the time when a patient decides to quit.
This barrier can be manifested in several ways including long waits for appointment times, distance needed to travel to access a provider, and limited availability of physician appointments outside of typical working hours. Additionally, many primary care physicians report insufficient time within the context of routine office appointments as a key barrier in being able to effectively address tobacco use with their patients.
To bridge this gap in care, in 2017 the US Centers for Medicare & Medicaid Services issued an informational bulletin encouraging states to “facilitate easier access to medically necessary and time-sensitive drugs for Medicaid beneficiaries,” including smoking cessation medications.
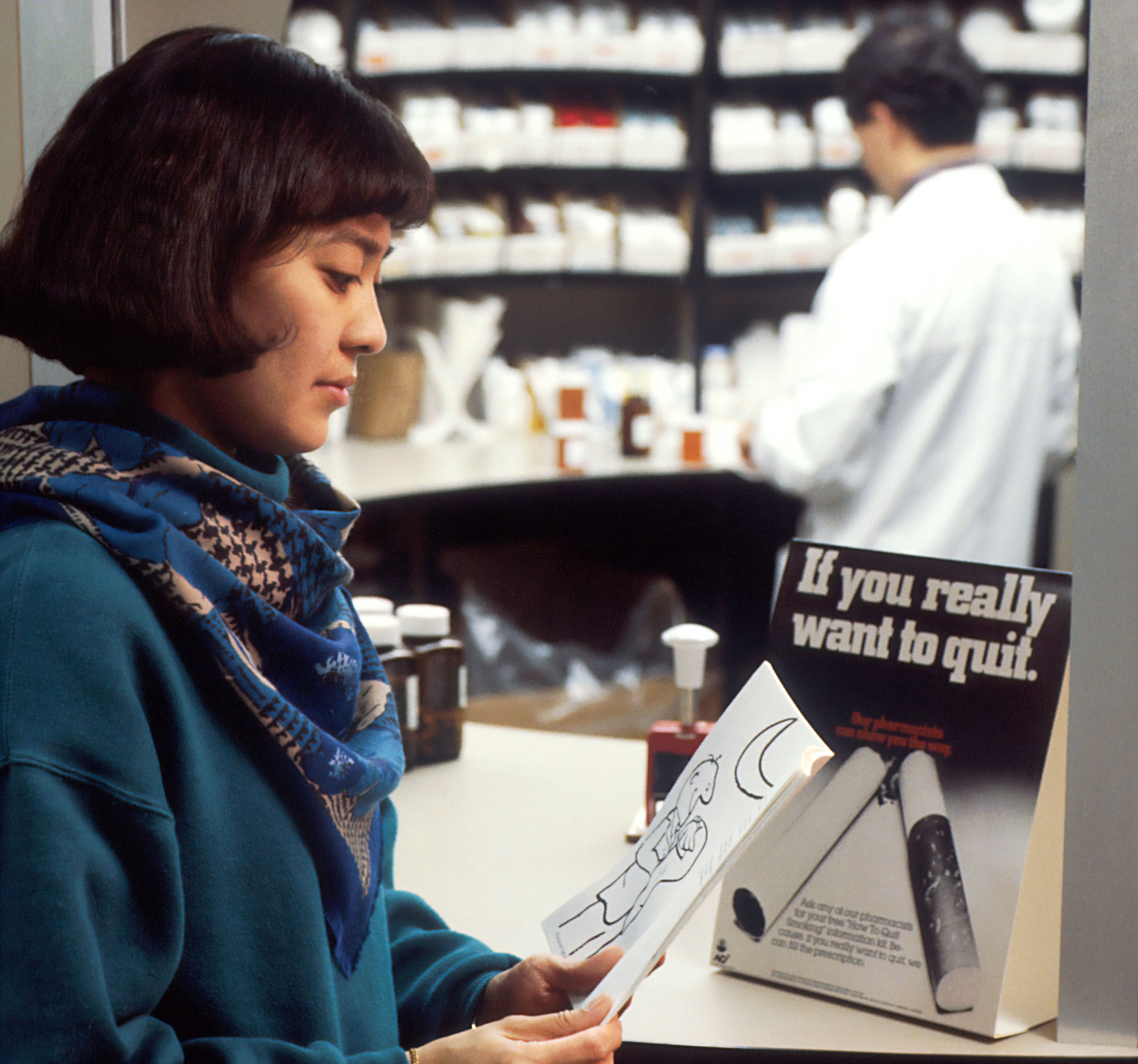
More than 90% of Americans live within five miles of a community retail pharmacy,[2] and most are open evenings and weekends. Importantly, the ability to walk into a pharmacy without an appointment allows tobacco users to initiate action the moment they feel the desire to quit, a moment that might pass if they must wait for an appointment with a physician.
Currently, a dozen states in the US have statutes or legislation permitting pharmacists to prescribe some or all FDA-approved pharmacotherapy for tobacco cessation.[3] These include New Mexico, where pharmacists have had prescriptive authority for this category of medications since 2004, Arizona, Arkansas, California, Colorado, Idaho, Indiana, Iowa, Maine, Missouri, Oregon, and West Virginia. Most of these states have minimum tobacco cessation education requirements for pharmacists who wish to prescribe, and the cessation protocols require (a) patient screening, (b) specific intervention components, and (c) documentation requirements, which collectively help to promote positive outcomes and enhance patient safety. It is notable that no negative reports related to pharmacist-prescribed cessation therapy have occurred in New Mexico across 15 years of protocol existence.
But how effective are pharmacists in helping patients quit? Several studies have shown that tobacco quit rates achieved when pharmacists prescribe cessation medications and provide counseling are similar to rates achieved by other healthcare professionals.[4] Importantly, in a study based in New Mexico, more than one third of patients assisted were non‐white, and 53.4% did not have health insurance,4 suggesting that pharmacists are effective in reaching vulnerable and uninsured populations.
Given that only 7.4% of smokers are successful when quitting unassisted,1 pharmacists could play an important role in enhancing quit rates. Pharmacies may also provide more cost-effective access to smoking cessation therapy.[5]
Physician burn-out, which is being at least partially driven by increased workloads, is a serious and growing challenge for the healthcare community.[6] Collaboration between physicians and pharmacists with respect to prescribing smoking cessation therapy, could achieve two beneficial goals of reducing demands on physicians’ time while increasing access to therapy that can help those motivated to quit smoking succeed in this difficult endeavor.
Physicians could benefit themselves and their patients by learning about options in their states to collaborate with pharmacists in the area of smoking cessation therapy and sharing appropriate information with patients regarding the role that pharmacists can play in helping them reach their quitting goals.
New digital solutions will also enable patients and providers to find a pharmacist who can prescribe smoking cessation therapy. Work is currently ongoing to launch a website that can help patients find a pharmacy near them that prescribes smoking cessation therapy, similar to the birthcontrolpharmacies.com project that has helped connect women with pharmacists who can prescribe birth control.
Although 2021 has already started, it’s not too late to resolve to quit smoking. Physicians and patients alike should know that, in some states, the local pharmacist can be a valuable and accessible resource for achieving this important but challenging goal.
Physicians in states that don’t yet permit pharmacists to prescribe smoking cessation therapy are encouraged to consider recommending this approach to their state health officials and legislators. Quitting smoking is difficult, and those who seek to do so deserve as much support as the healthcare community and our elected leaders can provide.
Karen Hudmon, DrPH, is a Professor of Pharmacy Practice at Purdue University.
Katy Ellis Hilts, PhD, is a Postdoctoral Fellow at the Indiana University School of Nursing.
References
[1] Babb S, Malarcher A, Schauer G, Asman K, Jamal A. Quitting smoking among adults - United States, 2000-2015. MMWR Morb Mortal Wkly Rep. 2017;65(52):1457e1464.
[2] American Lung Association. Indiana’s standing order for tobacco cessation: A case study. Available at: https://www.lung.org/getmedia/a673abfe-eb7e-4801-a374-01724df6ca6c/standing-order-indiana-case-study-final.pdf
[3] National Alliance of State Pharmacy Associations. Pharmacist prescribing: Smoking cessation aids. Available at: https://naspa.us/resource/tobacco-cessation/
[4] Adams AJ and Hudmon KS. Pharmacist prescriptive authority for smoking cessation medications in the United States. J Am Pharm Assoc. 2018;58(3):253-257. doi: 10.1016/j.japh.2017.12.015
[5] Csikar JI, Douglas GV, Pavitt S, Hulme C. The cost-effectiveness of smoking cessation services provided by general dental practice, general medical practice, pharmacy and NHS Stop Smoking Services in the North of England. Community Dent Oral Epidemiol. 2016;44:119e127
[6] Scheepers R, Silkens M, van den Berg J, Lombarts K. Associations between job demands, job resources and patient-related burnout among physicians: results from a multicentre observational study. BMJ Open. 2020;10(9):e038466. Published 2020 Sep 24. doi:10.1136/bmjopen-2020-038466





