Article
Intra-Articular Hyaluronic Acid Injections for Treating Symptomatic Osteoarthritis of the Knee
A meta-analysis provides evidence that hyaluronic acid injections improve pain symptoms and function in patients with symptomatic knee osteoarthritis.
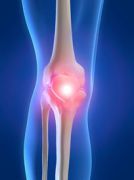
A study sponsored by the Hyaluronic Acid Viscosupplementation Coalition (HAVC), which is “a collaborative of hyaluronic acid injection marketers,” found that intra-articular hyaluronic acid (HA) injections significantly improve pain symptoms and function in patients with symptomatic knee osteoarthritis.
The authors of “US-Approved Intra-Articular Hyaluronic Acid Injections are Safe and Effective in Patients with Knee Osteoarthritis: Systematic Review and Meta-Analysis of Randomized, Saline-Controlled Trials, published in Clinical Medicine Insights: Arthritis and Musculoskeletal Disorders, reviewed data from 29 randomized controlled trials involving more than 4,800 patients with osteoarthritis of the knee who received intra-articular hyaluronic acid injections (IAHA).
Main inclusion criteria were “injection of a US-approved HA product, randomized, saline-control study design, primary diagnosis of knee OA, identical treatment and follow-up conditions between IAHA and saline-control groups, and at least one extractable efficacy or safety outcome.”
The authors stratified efficacy data into two post-injection time windows: 4—13 weeks and 14–26 weeks, and calculated two separate effect size statistics in each time window: pre-treatment to post-treatment standardized mean difference (SMD) for IAHA, and SMD for IAHA vs. saline control.
They reported that IAHA injection resulted in “very large treatment effects for knee pain and knee function compared to pre-injection values,” with SMD for knee pain of 1.37 at 4—13 weeks and 1.14 at 14–26 weeks (both P < 0.001). Treatment effects for knee function were slightly lower, with SMDs of 1.16 and 1.07, respectively (both P < 0.001).
When compared to saline controls, IAHA injection produced SMD of 0.43 at 4—13 weeks and 0.38 at 14–26 weeks for knee pain (both P < 0.001), and SMD of 0.34 (4—13 weeks) and 0.32 (14–26 weeks) for knee function (both P < 0.001).
The authors reported “no statistically significant differences between IAHA and saline controls for any safety outcome,” with all reported serious adverse events unrelated to treatment.
In their discussion of these results, the authors wrote that their findings “can be best characterized by a very large treatment effect of US-approved IAHA injections on knee pain and function between 4 and 26 weeks and, after statistically adjusting for saline-control improvements, a medium treatment effect with US-approved IAHA during this same period.”
They also acknowledged the study had excluded patients with end-stage OA of the knee, among several other limitations, and that “efficacy outcomes were inconsistent across studies and publication bias was evident for knee pain outcomes.”
The authors concluded that these results confirm that “intra-articular injection of US-approved HA products is safe and efficacious in patients with symptomatic knee OA.
In a news release that accompanied publication of the article, Mark A. Snyder, MD, an orthopedic surgeon from the TriHealth Orthopedic and Spine Institute in Cincinnati, OH, said the study results are not unexpected and are “consistent with what I and many other physicians have clinically observed for many years — HAs have been found to be safe, can help relieve knee pain from osteoarthritis, and are appropriate treatment for people with mild to moderate forms of the disease.”
These study results offer an interesting contrast to the recommendations of American Academy of Orthopaedic Surgeons (AAOS) published earlier this year. In “Treatment of Osteoarthritis of the Knee: Evidence-based Guideline”, the AAOS said that it “cannot recommend using hyaluronic acid for patients with symptomatic osteoarthritis of the knee,” ranking the evidence supporting this assertion as “strong.”

Real-World Study Confirms Similar Efficacy of Guselkumab and IL-17i for PsA


