Knee Injury in a 17-Year-Old Football Player
Author(s):
A slip on the grass sidelined a young football player 6 weeks after he sustained a complete tear of his medial collateral ligament. Learn how he added insult to the injury.

A 17-year-old football player sustained a knee injury during practice drills when another player rolled into the lateral side of his right knee. He was examined promptly and had normal Lachman and posterior drawer test results and normal tibiofemoral step-off at 90° of flexion. However, he demonstrated significant laxity to valgus stress testing at both 0° and 30° of flexion.
Plain radiographs showed normal results. A diagnosis was made of a complete tear of the player’s medial collateral ligament (MCL), and he was treated with several weeks of bracing and aggressive quadriceps strengthening.

The patient returned to play about 6 weeks after the injury. After about 1 more week, during a “grass drill,” his right foot gripped the turf firmly during a rolling maneuver and a forced external rotation moment was applied to his right tibia. The patient experienced sudden increased discomfort in the right lower extremity.
Sagittal (top) and coronal (bottom) MRI scans were obtained. What do they show?
What is your diagnosis?
Find the answer on the next page.
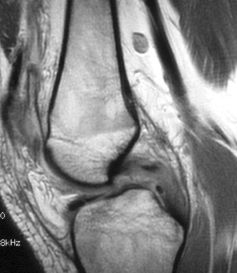
The patient had a tear of the posterior cruciate ligament (PCL) as well as of the MCL.The sagittal MRI scan (right) shows an intrasubstance tear of the PCL; the T2-weighted image demonstrates interstitial edema of the mid portion of the ligament, suggesting acute injury, with posterior translation of the tibia on the femur.The coronal image (below) shows edema and thickening of the midsubstance of the MCL.
The PCL is the primary restraint to posterior translation of the tibia on the femur.1 It also is a econdary restraint to valgus, varus, and external rotation stress to the knee joint.2The PCL most often is injured when a posterior-directed force is applied to the proximal tibia, as may occur in a dashboard injury. PCL injury also may result from both hyperextension and hyperflexion stress.3
Because the PCL is a secondary restraint to varus and valgus stress, severe injuries to the MCL or lateral collateral ligament may be accompanied by PCL ompromise. In addition, because the PCL helps resist external rotation of the tibia on the femur, torsional movements-especially significant external rotation of the tibia-may result in PCL violation. This “twisting” noncontact mechanism is especially common in patients participating in sports activities.4,5 Torsional PCL rupture may be seen in a ballplayer who suddenly changes direction away from the vulnerable knee, thereby externally rotating his body and femur on a fixed lower leg.5 This net external rotatory force on the tibia may cause failure of PCL fibers.
Sustaining a significant injury to his MCL about 2 months before presenting with this injury rendered our patient’s PCL more vulnerable to injury. In addition, his PCL may have been already somewhat compromised because of the initial valgus injury. However, both the posterior drawer and tibiofemoral step-off test results were normal after the first insult, reflecting minimal if any PCL violation during the index injury. The MCL was reinjured during the subsequent twisting injury because this ligament’s posterior fibers experience strain under external rotatory stress.
The posterior drawer test, which evaluates the femorotibial step-off, is the most sensitive test for making a diagnosis of PCL injury.6 To perform the posterior drawer test, the examiner places the patient’s knee at about 90° of flexion and applies a posterior force to the proximal tibia (photograph, left). The amount of posterior tibial translation and the quality of the end point are assessed.
PCL injuries are classified according to the amount of increased posterior translation (compared with the contralateral normal knee) determined by this test: grade 1 injuries, 5 mm or less, and grade 2 injuries, 1 cm or less; grade 3 injuries demonstrate greater than 1 cm of posterior tibial excursion. Because the tibial plateau normally rests about 1 cm anterior to the femur at 90° of flexion, grade 2 instability exists when the anterior plateau can be pushed “flush” to the femoral condyles; grade 3 injuries exhibit tibia translation posterior to the femoral condyles.
The medial ligamentous complex is composed mainly of the superficial and deep MCL and the posterior oblique ligament (POL).The MCL is the primary medial stabilizer of the knee to valgus stress,7 especially in slight knee flexion.The POL, a thickened capsular condensation immediately posterior to the MCL, confers resistance to valgus stress in extension. As was seen in our patient, instability at both 30° of flexion and in extension denotes violation of both the MCL and POL. Medial-side knee injuries are graded according to the amount of medial joint opening when valgus stress is applied at both 30° of flexion and in extension.8 Valgus opening of 0 to 5 mm at 30° of flexion indicates a grade 1 MCL lesion; 6 to 10 mm opening denotes a grade 2 injury; more than 10 mm of opening means that the MCL is fully torn. Medial joint opening in extension reflects POL injury; the same grading system applies.
Treatment of patients with isolated injuries to the medial ligamentous complex usually is conservative; bracing is used to promote ligamentous healing. However, grade 3 MCL injuries in the presence of a concomitant cruciate injury may not heal reliably and may be best treated with repair or reconstruction.9,10
Treatment of patients with PCL injuries is somewhat controversial. Most authors recommend conservative treatment for isolated grade 1 or 2 injuries.11-13 Others suggest operative treatment for younger, more athletic persons,14 those with higher-grade injuries,15 and those who sustained a PCL injury in combination with another ligamentous injury.16 Some evidence suggests that, unlike the anterior cruciate ligament, the PCL has some ability to heal, particularly when it is immobilized in extension.17 Despite immobilization, some persistent posterior instability usually remains. Most surgeons reserve PCL reconstruction for grade 3 injuries and most grade 2 injuries that are associated with a significant collateral ligament injury.
Cadaver studies suggest that posterior translation of the tibia on the femur is associated with increased contact pressures of the patellofemoral and medial compartments.18 Thus, if the normal posterior tibial step-off can be restored through surgery, more normal knee kinematics may result and, in theory, the onset of degenerative changes may be delayed.
Our patient was treated with a trial of immobilization in extension for 3 weeks and then with a quadriceps-strengthening program. However, he demonstrated significant persistent instability because of laxity of both the PCL and the MCL. Consequently, he elected to undergo surgical repair. At surgery, his examination under anesthesia revealed grade 3 PCL insufficiency as well as significant laxity to valgus stress at both 30° degrees of flexion and in extension. An endoscopic PCL reconstruction that used allograft tissue was performed in concert with medial ligamentous reconstruction. Allograft augmentation of the MCL was necessary along with POL advancement to restore medial-side ligamentous competence.
At about 1 year postoperatively, the patient indicated that he had no overt symptoms of instability. However, he had “retired” from organized football.
This case was submitted by John D. Kelly IV,MD, associate professor and vice chair in the department of orthopedic surgery at Temple University School of Medicine, Sports Medicine, in Marlton, New Jersey.
References:
1. Butler DL, Noyes FR, Grood ES. Ligamentous restraints to anterior-posterior drawer in the human knee: a biomechanical study. J Bone Joint Surg. 980;62A:259-270.2. Van Dommelen BA, Fowler PJ. Anatomy of the posterior cruciate ligament: a review.Am J Sports Med. 1989;17:24-29.3. Cooper DE. Clinical evaluation of posterior cruciate ligament injuries.Sports Med Arthroscopy Rev. 1999;7:243-252.4. Rubinstein RA, Shelbourne KD. Diagnosis and treatment of PCL injuries. Operative Techniques in Sports Medicine. 1993;1:99-103.5. Shelbourne KD, Nitz PA. Posterior cruciate ligament injuries. In: Reider B, ed. Sports Medicine: The School Age Athlete. Philadelphia: WB Saunders Co; 1991:318-319.6. Rubinstein RA Jr, Shelbourne KD, McCarroll JR, et al. The accuracy of the clinical examination in the setting of posterior cruciate ligament injuries.Am J Sports Med. 1994;22:550-557.7. Warren RF, Marshall JL, Girgis F. The prime static stabilizer of the medial side of the knee. J Bone Joint Surg. 1974;56A:665-674.8. Hughston JC, Andrews JR, Cross MJ, Moschi A. Classification of knee ligament instabilities, part I: the medial compartment and cruciate ligaments. J Bone Joint Surg. 1976;58A:159-172.9. Larson RL. Combined instabilities of the knee. Clin Orthop. 1980;147:L68-L75.10. O’Donoghue DH. Reconstruction for medial instability of the knee. J Bone Joint Surgery. 1973;55A:941-955.11. Parolie JM, Bergfeld JA. Long-term results of nonoperative treatment of isolated posterior cruciate ligament injuries in the athlete.Am J Sports Med. 1986;14:35-38.12. Fowler PJ, Messieh SS. Isolated posterior cruciate ligament injuries in athletes. Am J Sports Med. 1987;15:553-557.13. Torg JS, Barton TM, Pavlov H, Stine R. Natural history of the posterior cruciate ligament-deficient knee.Clin Orthop. 1989;246:208-216.14. Noyes FR, Barber SD. Allograft reconstruction of the anterior and posterior cruciate ligaments: report of ten year experience and results. In: Heckman JD, ed. Instructional Course Lectures. Vol 41. Rosemont, Ill: American Academy of Orthopaedic Surgeons; 1993;381-396.15. Veltri DM, Warren RF. Isolated and combined posterior cruciate injuries. J Am Acad Orthop Surg. 1993;1:67-75.16. Fanelli GC, Giannotti BF, Edson CJ. The posterior cruciate ligament arthroscopic evaluation and treatment. Arthroscopy. 1994;10:673-688.17. Shelbourne KD, O’Shea JJ. Natural history of PCL injuries. Sports Med Arthroscopy Rev. 1999;7:235-242.18. MacDonald P, Miniaci A, Fowler P, et al. A biomechanical analysis of joint contact forces in the posterior cruciate deficient knee. Knee Surg Sports Traumatol Arthrosc. 1996;3:252-255.





