Article
Long-Term Weight Control Linked to Better Late Life Heart Health
Author(s):
Weight from age 25 onwards has been linked to the risk of more or less heart damage, as measured by levels of the protein troponin, underscoring the importance of long-term weight control.

Chiadi Ndumele, MD, MHS
Maintaining a healthy weight long-term can have an even bigger positive effect on heart health than what was already believed, according to new clinical trial analysis.
A study from Johns Hopkins, led by Chiadi Ndumele, MD, MHS, the Robert E. Meyerhoff assistant professor of medicine at the Johns Hopkins University School of Medicine and a member of the Johns Hopkins Ciccarone Center for the Prevention of Heart Disease, found that obesity and escalating weight from young adulthood onward increases the long-term toxic effects of adiposity, and thus the likelihood of myocardial damage.
“We’re finding that people’s weight from age 25 onwards is linked to the risk of more or less heart damage, as measured by levels of the protein troponin, later in life, which underscores the likely importance of long-term weight control for reducing heart disease risk,” Ndumele said in a statement. “What our findings suggest is that even in the absence of such heart disease risk factors as high blood pressure, diabetes or kidney disease, the number of years spent obese or overweight contributes to the higher likelihood of heart damage.”
Nduemele and colleagues examined data on 9062 Atherosclerosis Risk in Communities (ARIC) study participants from visit 4 of the study (1996—1999), each with a body mass index (BMI) of ≥18.5 kg/m2 and no previous indications of cardiovascular disease. Visit 4 BMI was defined as the “current” BMI and divided into 3 categories: normal weight, overweight, and obese.
With regard to age at each time period, they compared those data with those logged at visit 1 (1987—1989) and the self-reported weight at age 25 years. Mean age at visit 4 was 63 years. At the 4th visit, 41.3% of participants (n = 3748) were classified as overweight and 35.1% as obese (n = 3184).
From visit 1 to visit 4, overall 23% of participants experienced weight increases, while 5% showed decreases, and the remaining 72% remained about the same.
Credit: Johns Hopkins
Data revealed 7% of participants (n = 623) had increases ≥14 ng/L in high-sensitivity cardiac troponin T (hs-cTnT) concentrations, used to reflect subclinical myocardial damage, by visit 4. There were associations found within each current BMI category between previous excess weight and increased hs-cTnT—with the strongest links found between those with obesity at both age 25 and visit 4 (odds ratio [OR], 3/85; 95% CI, 2.51—5.90).
The investigators also calculated obesity duration in years, and excess BMI-years, defined as the product of mean BMI over all the AIRC time points multiplied by follow-up duration. BMI-years among participants ranged from —274 to 1205.
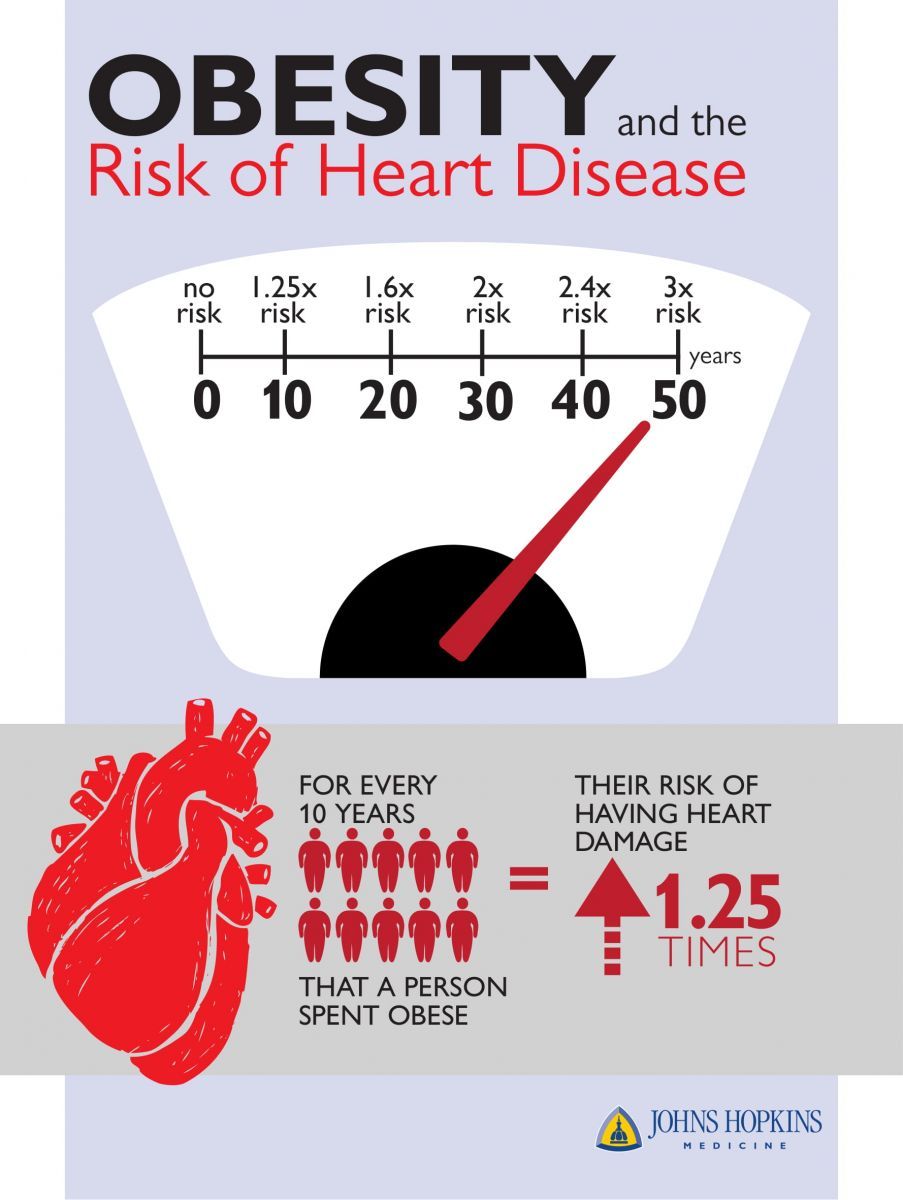
They found that each obesity duration of 10-years or longer was associated with a 1.25-fold increase in hs-cTnT (OR, 1.26; 95%CI, 1.17—1.35) when taking into account hypertension, and diabetes and kidney disease. Each 100 higher BMI-years was progressively associated with a 21% risk of increases in hs-cTnT (OR, 1.21; 95% CI, 1.14–1.27).
“It’s challenging to effectively communicate future risk to young people who seem perfectly healthy and at the prime of their lives,” Ndumele said. “A measurement like excess BMI-years could be developed and tested as a way of communicating risk to young and middle age people to reduce their long-term risk of cardiovascular disease by maintaining a healthy weight.”
There is evidence that even after being obese or overweight for decades, Ndumele said, that losing weight could help reduce hs-cTnT levels enough to give the heart time to heal, however, more studies must be conducted to understand the extent to which the heart can repair the damage, some of which may be permanent.
More than one-third of adult Americans are obese, according to data from the Centers for Disease Control and Prevention. Cardiovascular disease as an underlying cause of death, totals almost 801,000 deaths annually in the United States, according to the American Heart Association.
The study, “Weight History and Subclinical Myocardial Damage,” was published in Clinical Chemistry.
Related Coverage >>>
Women Less Likely to Be Treated for Heart Attack Symptoms
Ustekinumab Shown to Reduce Aortic Inflammation
FDA Rejects Apricus Biosciences' Alprostadil Erectile Dysfunction Cream





