Article
Low back pain contributors: Defining a role for biomechanical deficiencies
Although low back pain (LBP) may be attributed to a variety of known vertebral disorders (eg, fractures, infections, tumors, and hernias), a definitive diagnosis often remains elusive.1 Biomechanical deficiencies of the lumbar spine may be a contributor, according to students at the University of Southern California's Musculoskeletal Biomechanics Research Laboratory (MBRL), and they are conducting research to determine what role the deficiencies may play in an effort to identify improved rehabilitation interventions.
Although low back pain (LBP) may be attributed to a variety of known vertebral disorders (eg, fractures, infections, tumors, and hernias), a definitive diagnosis often remains elusive.1 Biomechanical deficiencies of the lumbar spine may be a contributor, according to students at the University of Southern California's Musculoskeletal Biomechanics Research Laboratory (MBRL), and they are conducting research to determine what role the deficiencies may play in an effort to identify improved rehabilitation interventions.
A series of experiments that could enhance understanding of how the lumbar neuromuscular stabilizing system is impaired in persons with LBP are being performed by MBRL student George J. Beneck, PT. In a pilot study for his thesis, "Lumbar Paraspinal Morphology, Activation, and Fatigability in Persons With Chronic Low Back Pain," Beneck used MRI to collect data from subjects who had a herniated disk and presented with unilateral LBP. There was 11% lower muscle volume (in both nonprocessed and normalized data) in the multifidus spinae muscles on the patients' painful side than on the nonpainful side.
The multifidus spinae is an extremely thin, deep extensor muscle that connects directly to the 5 lumbar vertebrae (L1-L5) of the lower back region. The tendinous nervous tissue that makes up the multifidus serves to stabilize and protect the vertebral joints that are responsible for supporting the weight of the upper body. When the morphology (size and structure), activation (timing), or ability of the multifidus to resist fatigue is compromised, the resultant deficits in muscular stability and intervertebral control place the spine at risk for injury and pain.
Separate pilot studies involved the use of electromyographic (EMG) measures designed to compare the latency and fatigability of the multifidus muscle in subjects who have LBP with those in non-LBP controls. In the first EMG base study, longer latencies were demonstrated in the persons with LBP during performance of a load-release trunk perturbation task that was recorded via 3D motion.
A second study relied on MATLAB computer processing of EMG data collected while the subjects maintained their trunk on the horizontal against gravity. A higher rate of decline of the normalized median frequency of the deep fibers seen in the subjects with LBP indicates somewhat greater multifidus fatigability.
The experimental subjects in Beneck's full-scale studies will include both women and men older than 18 years whose LBP has been chronic and responsible for recurring episodes (minimally once per year) of sufficient intensity to have resulted in absenteeism (minimally 3 consecutive days) from work or school. The experimental group will not contain subjects whose medical history suggests a definitive cause of their LBP. As in the pilot studies, both MRI and EMG measures will be used to collect data on the multifidus of experimental subjects and healthy controls.
Beneck hypothesizes that the data will confirm his preliminary findings indicating that the multifidus in persons who present with LBP will be smaller, slower to respond to neural activation, and more susceptible to fatigue than that in healthy persons. "Beneck's work has the potential to make a significant mark on musculoskeletal rehabilitation and, in particular, spine rehabilitation," said Christopher Powers, PhD, PT, his MBRL advisor.
Correlations have been suggested between morphological abnormalities (eg, leg length discrepancies) on the basis of asymmetrical static pelvic alignment and the uneven spinal tissue loading that is thought to be the cause in some cases of LBP. Dynamics-based factors, such as diminished hip muscle performance, also could be responsible for the abnormalities in the lumbopelvic region that tend to result in LBP. "Despite the vast amount of research exploring the factors related to LBP, the relationship between lower extremity impairments and low back problems remains relatively uncharted," said MBRL PhD candidate John Popovich, DPT.
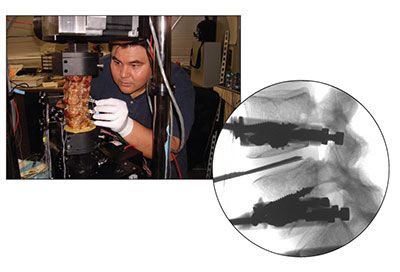
Popovich's dissertation, "Lumbopelvic Kinematics, Muscle Activation, and Lumbar Spine Load Sharing in the Presence of Diminished Hip Muscle Performance," will be the first comprehensive biomechanical investigation to address the relationships among diminished hip abductor muscle performance, pelvis position, and lumbar spine mechanics (Figure). The study is intended to test whether persons with diminished hip abductor performance (1) demonstrate greater peak amplitudes in frontal plane lumbopelvic kinematics, (2) select greater lumbopelvic muscle activation of the hip and trunk musculature, and (3) experience increased loading with increases in frontal plane motion and under combined loading conditions.
The projects that make up Popovich's dissertation include both cadaveric and human subject experimentation. The cadaveric study uses a 6 degrees of freedom material testing machine, instrumentation to measure loading to the lumbar facet joints and intervertebral disks, and a custom-designed apparatus capable of applying simulated loads to the spine.
Popovich is reticent to comment on the potential implications of his study until the data are fully analyzed. However, MBRL associate professor of clinical physical therapy Kornelia Kulig, PhD, PT, stated, "Popovich's work will begin to answer questions about the consequences of selective or global hip muscle weakness on lumbopelvic mechanics, and in that his work is innovative and relevant."
LBP is the second most common neurological ailment and the most common cause of job-related absenteeism in the United States.2 It accounts for nearly $100 billion in annual health care spending and lost productivity.3
1. Bloodworth D, Grabois M. Physical medicine and rehabilitation. In: Warfield CA, Bajwa ZH, eds. Principles and Practice of Pain Medicine. 2nd ed. New York: McGraw-Hill; 2004:273.
2. Office of Communications and Public Liaison, National Institute of Neurological Disorders and Stroke, National Institutes of Health. Low Back Pain Fact Sheet. 2003. Publication 03-516.
3. Luo X, Pietrobon R, Sun SX, et al. Estimates and patterns of direct health care expenditures among individuals with back pain in the United States. Spine (Phila Pa 1976). 2004;29:79-86.




