Article
Low Risk of Venous Thromboembolism with Tofacitinib
Author(s):
The JAK inhibitor tofacitinib presents a comparably low risk of venous thromboembolism to rheumatoid arthritis patients as do TNFi inhibitors, according to a new study.
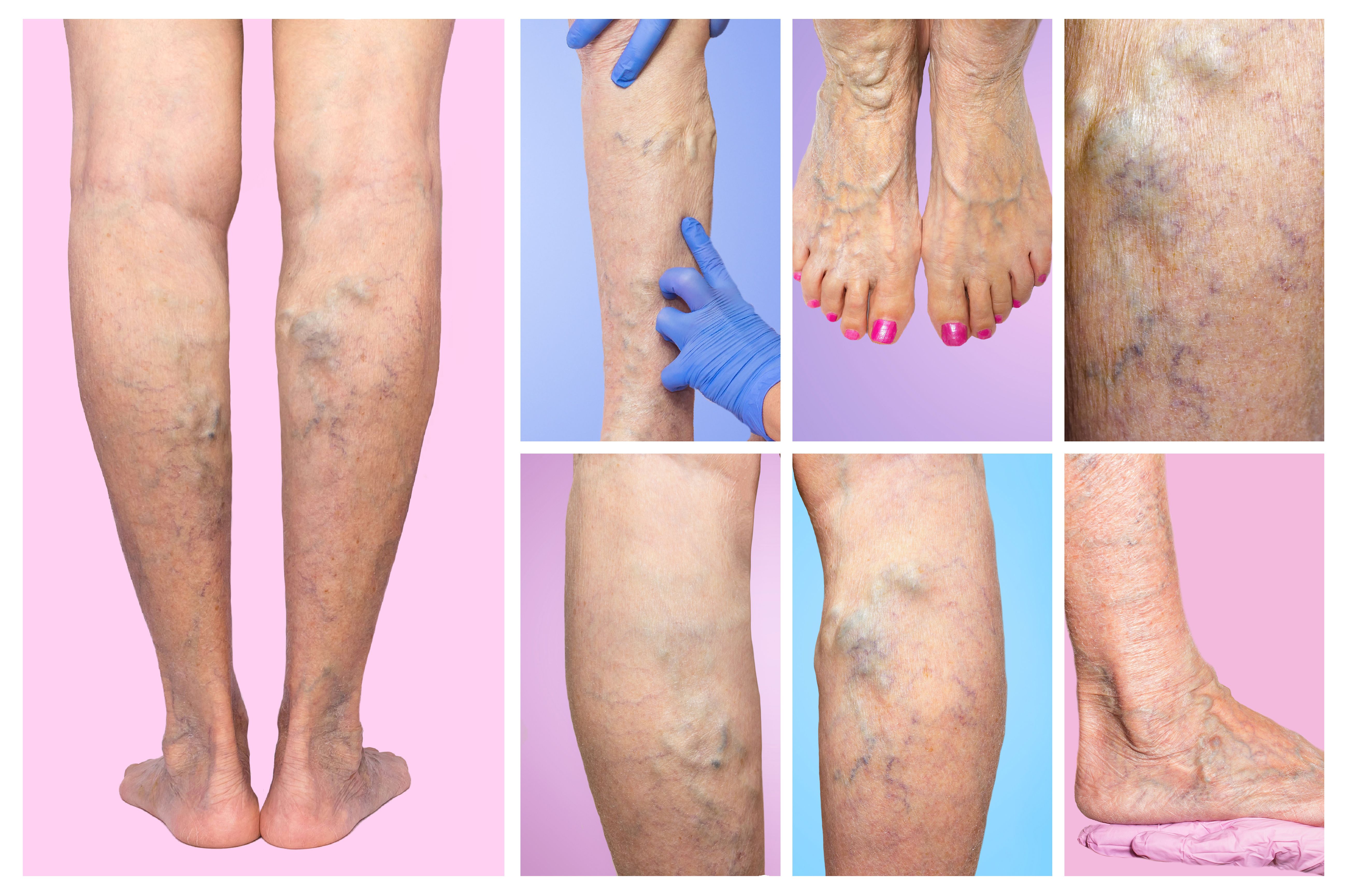
Lower limb vascular examination because suspect of venous insufficiency. (©Solarisys, AdobeStock.com)
The JAK inhibitor tofacitinib presents a comparably low risk of venous thromboembolism to rheumatoid arthritis patients as do TNFi inhibitors, according to a new study.
These findings, published in a recent Arthritis & Rheumatology issue, underscore the safety of using this therapy for patients with rheumatoid arthritis and other systemic autoimmune inflammatory disorders, investigators said.
“Our study adds important new data to the literature by providing preliminary reassurance regarding the safety of tofacitinib with respect to venous thromboembolism risk,” said study author Rishi Desai, Ph.D., an epidemiologist at Brigham & Women’s Hospital. “Our results provide timely information regarding the risk of a suspected adverse event for this important drug class in patient populations receiving routine care to help contextualize the risk-benefit tradeoffs.”
Overall, the incidence rate of venous thromboembolism has been reported to be approximately 2.4 times higher among rheumatoid arthritis patients, regardless of the treatment they receive. Consequently, researchers said, clinicians should maintain awareness of possible venous thromboembolism development with all patients in this group.
To determine how the risk of venous thromboembolism compared between tofacitinib and more traditionally used TNFi inhibitors, researchers conducted an observational study of 457,171 patients receiving both therapies. Venous thromboembolism occurred with 50,865 individuals. Within that group, a higher number of tofacitinib patients had received three or more nonbiological DMARDs and glucocorticoids at baseline, indicating they already had more active and longer-lasting rheumatoid arthritis.
Based on this study’s results, more occurrences of venous thromboembolism appeared within the tofacitinib group, but the amount was not statistically significant compared to the TNFi treatment group, researchers said. This outcome is also similar to the rate of venous thromboembolism seen among patients receptive baricitinib treatment, as well.
Ultimately, researchers said, while continued monitoring of JAK inhibitor venous thromboembolism risks is necessary, these findings can help rule out the possibility of a large increase in the incidence of pulmonary embolism or deep vein thrombosis among tofacitinib patients.
REFERENCE
Desai R, Pawar A, Weinblatt M, Kim S, Comparative Risk of Venous Thromboembolism in Rheumatoid Arthritis Patients Receiving Tofacitinib Versus Those Receiving Tumor Necrosis Factor Inhibitors: An Observational Cohort Study. Arthritis & Rheumatology (2018), doi: 10.1002/art.40798




