Publication
Article
Family Practice Recertification
More Comprehensive HIT Use Would Reduce Future Demand for Physicians
Author(s):
Even if health information technologies (HIT) were only fully implemented in less than a third of all primary care offices, the overall demand for physicians would still fall by nearly 10% due to increased efficiency.
Even if health information technologies (HIT) were only fully implemented in less than a third of all primary care offices, the overall demand for physicians would still fall by nearly 10% as a result of increased efficiency, according to research published in the November 2013 issue of Health Affairs.
In what they called the “most comprehensive review of the literature to date,” Jonathan P. Weiner, DrPH, director of the Johns Hopkins Center for Population Health IT in Baltimore, and researchers from the Johns Hopkins Bloomberg School of Public Health and the Commonwealth Fund pulled data from systematic reviews and individual studies published through June 2013 to estimate the impact a more widespread, comprehensive use of HIT would have on future patient demand for primary care physicians.
“The current knowledge base provides substantial evidence supporting the premise that consumer and provider IT systems will significantly affect the way office-based care is delivered in the future — which in turn will have a strong impact on future demand for physicians,” the authors wrote. “As such, future predictions of the adequacy of physician supply should take these changes into account.”
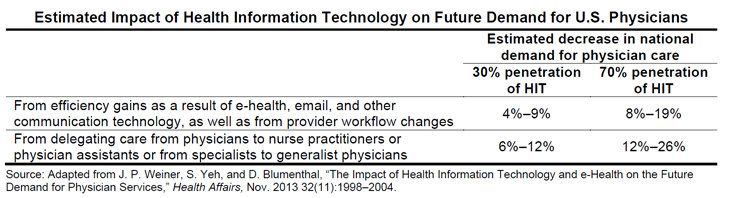
At the conclusion of their review, the researchers determined that if HIT — which include interoperable electronic health records (EHRs), clinical decision support, provider order entry, and online patient portals with secure messaging — were utilized by 30% of primary care physicians’ offices, the total patient demand for physicians would be reduced by 4-9% from efficiency gains and another 6-12% from the delegation of HIT-supported tasks from physicians to midlevel healthcare professionals, or from specialists to generalist physicians. In addition, the authors wrote that “the use of HIT could also help address regional shortages of physicians by allowing 12% of care to be delivered remotely or … in separate locations and at different points in time.”
Each of those estimated impacts would more than double if full HIT implementation expanded to 70% of physician offices, the investigators said.
But while roughly 72% of community-based physicians had adopted an EHR as of 2009, the study authors said comprehensive HIT use at even the lower threshold of 30% of primary care offices could take another 5 years, though they acknowledged “it is also possible that HIT adoption will not be widespread until later.”
Regardless of when widespread HIT adoption occurs, the researchers emphasized that “HIT and electronic health applications will likely change the shape of the healthcare workforce by raising efficiency; allowing more patient care to be provided by physician assistants and nurse practitioners, and by generalist rather than specialist physicians; and by increasing the opportunity for patients to receive care remotely.”






