Publication
Article
Internal Medicine World Report
Novel Hepatitis C Treatment Produces 'Out-of-the-ballpark' Cure Rates in Cirrhosis Patients
Author(s):
An oral, interferon-free regimen comprised of several agents cured hepatitis C in more than 90% of patients who also had liver cirrhosis, according to the results of an international study.
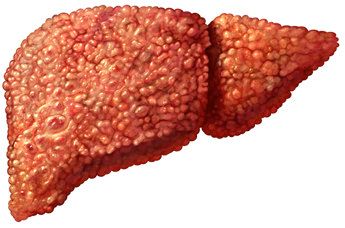
An oral, interferon-free regimen comprised of several agents cured hepatitis C in more than 90% of patients who also had liver cirrhosis, according to the results of an international study. Historically, hepatitis C cure rates among cirrhosis patients are lower than 50%.
In addition to high rates of sustained virologic response, drug discontinuations due to adverse events were infrequent, according to the research published in the New England Journal of Medicine. Fred Poordad, MD, lead author of the study and a clinical professor of medicine at the School of Medicine at the University of Texas Health Science Center at San Antonio, presented the data at the 2014 International Liver Congress held in London in April.
“These are out-of-the-ballpark response rates, not on the same planet as interferon,” Poordad said in a statement. “The reason this study is so profound is because interferon is not tolerated, nor is it safe in many people with cirrhosis. Many of the patients with cirrhosis in this study were not even eligible to be treated with interferon.”
For the study, Poordad and his co-authors examined 380 patients between the ages of 18 and 70 years old at 78 hospitals and health centers in Europe and North America, including sites in Canada, England, Germany, Spain, and the US. The patients either received 12 or 24 weeks of treatment with ABT-450/r—ombitasvir, a once-daily dose of 150 mg ABT-450, 100 mg ritonavir, and 25 mg ombitasvir; twice-daily 250 mg dasabuvir; and ribavirin administered according to body weight.
Of the 208 patients who received 12 weeks of treatment, 191 (91.8%) were cured at the end of intervention. Of the remaining 172 patients who received 24 weeks of treatment, 165 (95.9%) were hepatitis C virus (HCV) free at the end of intervention.
“Patients with advanced liver disease can now be cured of their hepatitis with a very well-tolerated and short regimen,” Poordad concluded in response to the results.
The most common adverse events were fatigue, which was reported in 32.7% of the 12-week group and 46.5% of the 24-week group; headache in 27.9% and 30.8%, respectively; and nausea in 17.8% and 20.3%, respectively. Although adverse events were reported in about 91% of each group, just 2.1% of patients discontinued treatment as a result.
According to Poordad, the researchers will catalogue patient blood samples for 3 years after therapy, though they have noticed no long-term, late relapses thus far.
The drug combination used in the study is manufactured by biopharmaceutical company AbbVie and expected to hit the market as early as the end of 2014.






