Article
Novel Mechanisms in Urticaria Development
Author(s):
Researchers have been investigating potential mechanisms involved in the generation of urticarial lesions, the role of IgE-targeting in allergic diseases, and the clinical characteristics of chronic spontaneous urticaria.
During the American Academy of Allergy, Asthma and Immunology’s 2015 annual conference in Houston, TX, Sarbjit S. Saini, MD, Associate Professor of Medicine at the Johns Hopkins University School of Medicine in Baltimore, MD, discussed the potential mechanisms involved in the generation of urticarial lesions, the role of IgE-targeting in allergic diseases, and the consequences of chronic spontaneous urticaria (CSU).
Acute urticaria is the predominant form of the condition, and its lifetime prevalence is around 20%. Chronic urticaria has a lower prevalence, around 1%, and affects more women than men (in approximately a 2:1 ratio). While acute urticaria is generally triggered by infections, food and drug allergens, and physical stimuli, the triggers for CSU are less well understood.
Saini highlighted the fact that CSU has an important autoimmune background. CSU patients have increased production of autoantibodies and higher incidence of thyroid and autoimmune diseases compared with healthy individuals. In the clinical setting, however, it is hard to differentiate between acute and chronic urticaria.
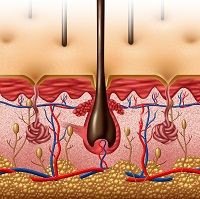
In 2002, Ying and collaborators demonstrated that CSU skin lesions have more infiltration of macrophages, mast cells, lymphocytes, and eosinophils than normal controls. Nevertheless, these differences are not very helpful in the differential diagnosis. To further characterize these lesions, Kay and collaborators have evaluated non-lesional and lesional skin from CSU patients. They have observed that non-lesional skin is not entirely normal, as there is increased infiltration of leukocytes and eosinophils.
On the other hand, lesional skin has increased expression of cytokines (IL-5, IL-33, TSLP). Saini emphasized that this increase in cytokines happens in the absence of allergens, reinforcing the idea that a native response occurs in patients with CSU. He suggested that this increase in cytokines expression might be related to the T helper cell 2 (Th2) response. He told the audience that other researchgroups have observed an important elevation in the expression of filaggrin protein and decreased pH in lesional skins. Additionally, an important depletion of basophils in the circulation has been observed in CSU patients. In a recent paper, Saini also demonstrated that the coagulation cascade is elevated in lesions of CSU patients.
Next, he discussed a conceptual model for the development of CSU. According to this model, various triggers affect skin mast cells, activating a cascade that involves the production of prostaglandin D2 (PgD2) and cytokines, and the recruitment of lymphocytes and eosinophils. Additionally, he mentioned that several autoantibodies have been identified in the development of the CSU, which led to the development of the autoimmune hypothesis.
For many years, CSU was considered a disease of mast cells number; however, Saini highlighted that the number of mast cells in the skin of CSU patients is normal, but that the release of histamine by theses cells is increased.
Finally, after presenting several studies that evaluated the mechanisms involved in the development of the disease, Saini concluded saying that CSU is a disease that involves mast cells release and a large infiltration by a variety of leukocytes in the skin. The cause of this increased release, still, remains a mystery. Additionally, he pointed out that variations in IgE levels have potential implications for the disease development and progression. Therapies that reduce IgE expression or interfere with its pathway could have beneficial effects on SCU.





