Article
Perceptions of Pain Education at Top-rated Medical Schools Conflict with Reality
Author(s):
Medical and nursing schools that reported extensively incorporating the topic of pain care into prelicensure curricula do not offer more robust pain management education programs than those indicating minimal or moderate pain course integration.
In a research poster presented at the American Pain Society 33rd Annual Scientific Meeting, held April 30, 2014, to May 3, 2014, in Tampa, FL, medical and nursing schools that reported extensively incorporating the topic of pain care into prelicensure curricula did not offer more robust pain management education programs than those indicating minimal or moderate pain course integration.
Within their “Pain Education at US Medical and Nursing Schools” study, Jennifer Mongoven, MPH; Heather M. Young, PhD, RN, FAAN; Ian Koebner, MSc, MAOM, LAc; and Scott M. Fishman, MD, of the Department of Anesthesiology and Pain Medicine and the Betty Irene Moore School of Nursing at the University of California, Davis, pointed out that most healthcare professional education programs in the US have not emphasized pain management in their curricula, despite the fact that approximately 100 million Americans suffer from chronic pain.
To gain insight on the current state of pain education in the United States, the research team distributed a Web-based survey to 64 medical and nursing schools selected from US News and World Report’s 2011 Best Graduate Schools rankings. Of those top-ranked institutions, 13 medical schools and 18 nursing schools responded to the survey.
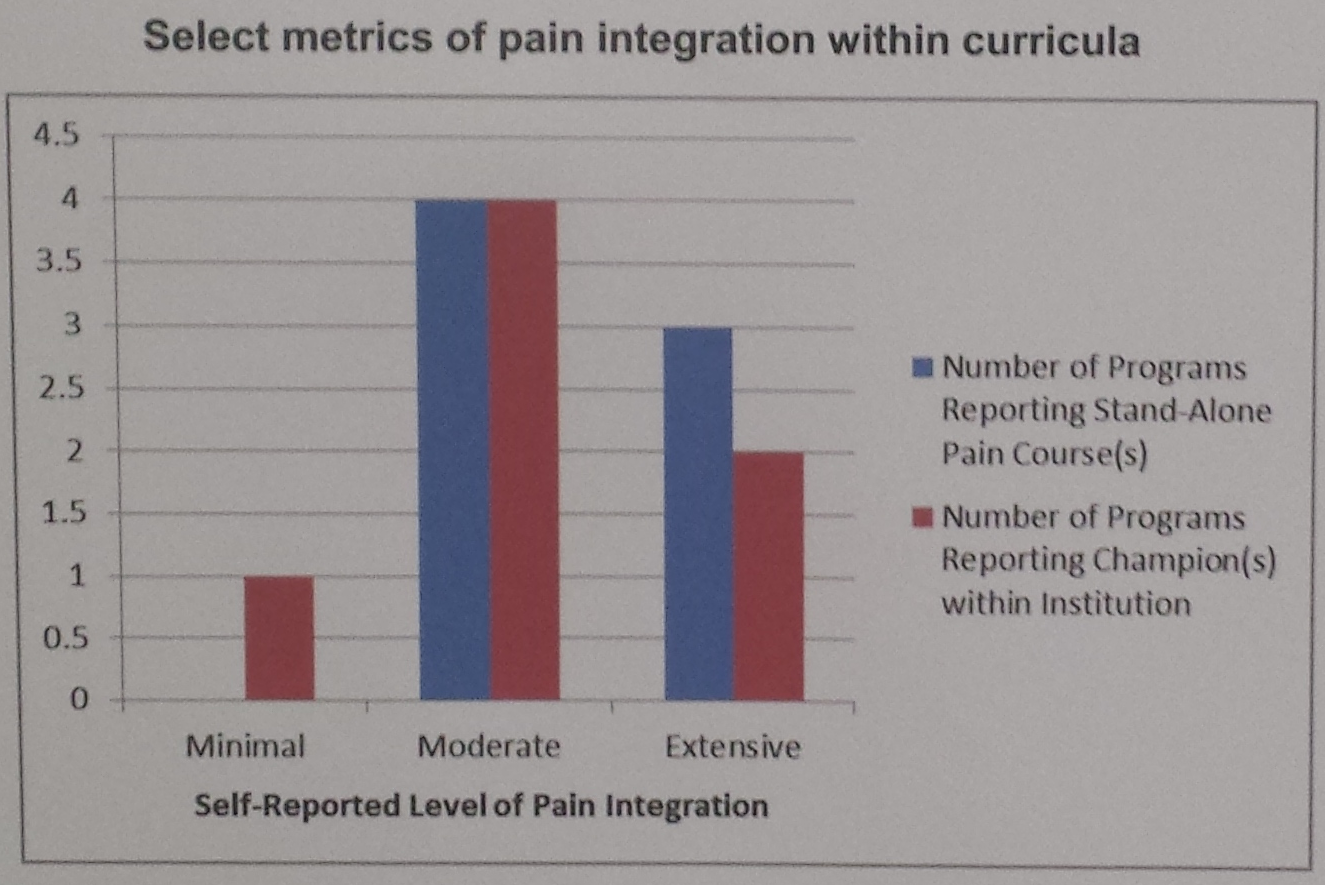
In the survey, responders were asked to rate how well their prelicensure programs incorporate pain into curricula on a 1-10 scale, with a score of 1 meaning pain is not covered at all and a score of 10 meaning pain management is covered extensively. Although the mean score across all 31 schools was 6.33, the researchers classified the individual programs into 3 categories based on the extent to which they reported integrating pain education: minimal, moderate, and extensive.
Among the 4 medical schools and 9 nursing schools that indicated extensive pain integration, “3 offered stand-alone courses in pain and reported an average of 4.5 other courses that incorporated the topic of pain,” the poster authors wrote. However, among the 7 medical schools and 10 nursing schools that specified only moderate pain incorporation, “4 reported stand-alone courses and averaged 5.3 additional courses;” therefore, “schools reporting extensive integration of pain did not appear to suggest a more robust pain management program than those reporting lower ratings,” they noted.
While some medical and nursing schools reported including pain management topics in a variety of mandatory and optional courses focused on pharmacotherapy, obstetrics, surgery, and palliative care, several others indicated limiting pain education to basic science courses. Still, the medical schools utilized clerkships as a mechanism for teaching pain care.
Taken altogether, the preliminary study findings “indicate pain is inconsistently incorporated into curricula for both nursing and medicine prelicensure programs (and) suggest a conflict may exist between the perceived and actual incorporation of pain management within curricula,” Mongoven, Young, Koebner, and Fishman concluded. Even so, they acknowledged, “more research is needed on how schools can easily assess and map the level of which the topic of pain management is incorporated into curricula.”




