Article
Physician Assistants: Growing in Number and Scope
Author(s):
The PA profession has grown nearly 54% in 7 years, particularly in specialties including surgery, emergency medicine, dermatology, and hospital medicine.
Editor’s note: This is a column by Dawn Morton-Rias, EdD, PA-C, President and CEO of the National Commission on Certification of Physician Assistants (NCCPA), the nation’s only certifying body for PAs. She has been certified as a PA for over 30 years, and has worked in family medicine, addictive medicine, GYN, and acute care for the homeless.Health care professionals and researchers interested in responding to this piece or similarly contributing to MD Magazine® can reach the editorial staff by submitting a request here.

Dawn Morton-Rias, EdD, PA-C, President and CEO, NCCPA
When I graduated from college over 30 years ago and told my parents that I was considering becoming a physician assistant (PA), my father asked me if I would be able to find work in this profession.
Today, PA is one of the jobs in greatest demand, ranking #3 on US News and World Report’s 100 Best Jobs list. The evaluation was based on whether the jobs “pay well, challenge us year after year, match our talents and skills, aren't too stressful, offer room to advance throughout our careers and provide a satisfying work-life balance. Whether the position is in demand is also a consideration.”
Changes and Growth in the PA Profession
This list portends well for the PA profession and may be one reason why the majority of new PAs have multiple job offers, that the number of PA programs is growing quickly (projected to go from 229 to 291 by 2021), and that competition for admission to these programs is at an all-time high.Physicians who are familiar with the scope of PA practice in their own organization or department may be surprised by how much the profession has changed since its inception.
The first physician assistant program began at Duke University 50 years ago to provide formal education to returning military medics who had clinical on the job training during the Vietnam War. They were educated to work alongside physicians in primary care settings.
From its military male-dominated roots, the profession has shifted to one that is majority female (68%) and has expanded into every specialty and clinical setting.
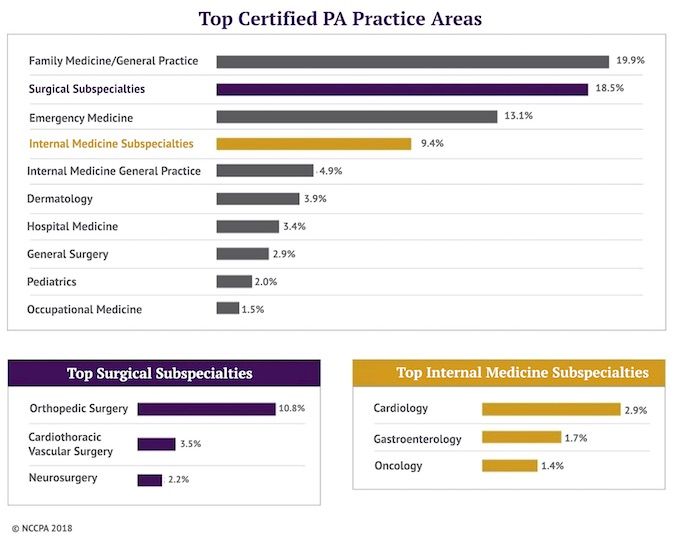
The 2017 Statistical Report on Certified PAs shows the impact that PAs are making on patient care. The profession has grown almost 54% in 7 years and the fastest growing areas are outside of primary care. For example, the fastest growing specialty for PAs is in surgery. The number of PAs working in surgical subspecialties has increased 70% since 2013.
Physician assistants are also in high demand in emergency medicine, dermatology, and hospital medicine. Additionally, PAs are starting to make inroads in specialties that have tremendous and growing need, such as psychiatry, hospice, and palliative care.
Physician Assistants in Underserved Areas
The statistical report also shows that the average physician assistant sees 73 patients a week, which translates to over 8.5 million patients per week, or 449 million patients each year. Clearly, they are a critical link between the public to the nation’s health care system.
Yet more PAs are needed, particularly in underserved and remote areas where physician recruitment and retention are challenged. Certified PAs have a long history of providing essential care in these areas, from remote regions like islands off of Alaska to Native American reservations, rural and frontier communities across America, prisons, inner city free clinics, extended care facilities, and nursing homes. Indeed, many of the patients treated by certified PAs are recipients of either Medicaid or Medicare.
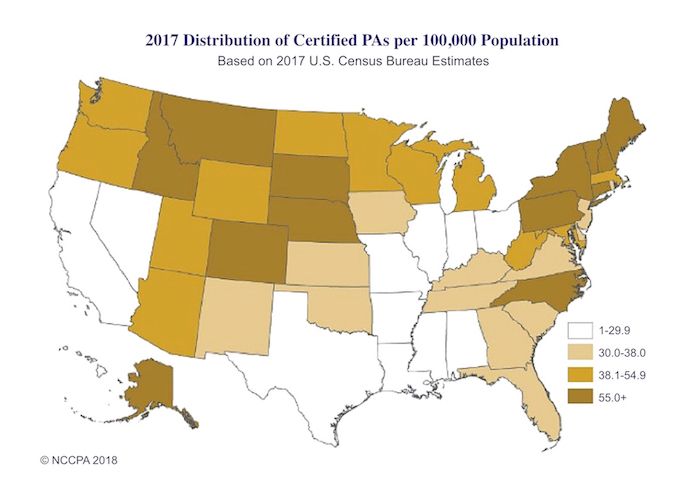
The greatest number of PAs tends to be in the populous states such as New York, California, Texas, and Florida. However, the top states ranked by concentration per 100,000 population include those with rural areas such as Alaska, South Dakota, Maine, and Idaho.
What services do physician assistants perform?
Although physician assistant services vary by specialty, certified PAs provide many of the same services as physicians, from completing physicals to prescribing medications, treating chronic comorbidities, performing procedures, and educating patients.
What qualifies PAs to provide these complex services, treat chronic illnesses, assist in surgery and even manage medications for the mentally ill?
PA education programs are highly competitive and most require applicants to have some prior health care experience. These programs are at the master’s degree level, averaging 26 months in length. The first-year averages 1,000 hours of didactic education followed by a second and sometimes even third year averaging 2,000 hours of clinical rotations.
After graduation, all PAs must pass the National Physician Assistant Certifying Exam to become certified and get a license in any of the 50 states and Washington, DC. PAs maintain certification like many physicians, through substantial CME and by passing an assessment every 10 years. Approximately 97% of PAs maintain certification throughout their career, and employers and the public rely on the PA-C credential as a measure of the physician assistant’s knowledge and skills.
PA scope of practice is determined both by state law and at the practice level in conjunction with the employer. Working closely with physicians, PAs continue to grow their experience and expand their delegated responsibilities.
As the population increases and baby boomers live longer with multiple comorbidities, the demand for services will continue its upward trend. Both the physician shortage and the need for more patients to be treated account for this huge increase in demand.
Just in the last 4 years, the number of PAs per 1,000 physicians has grown 23%. This increasing demand suggests that certified PAs are good for America’s health care needs.





