Article
Preventing “Sunset Glow†in Patients with Acute Uveitis from Vogt–Koyanagi–Harada Disease
Author(s):
A combination of mycophenolate mofetil and corticosteroid showed benefit.
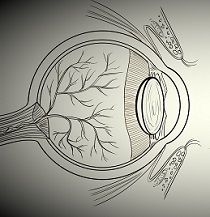
Vogt-Koyanagi-Harada disease (VKH) is a multisystemic disorder characterized by neurologic abnormalities, tinnitus, alopecia, and vitiligo as well as severe granulomatous panuveitis in both eyes. This autoimmune inflammatory condition is mediated by T cells that target melanocytes in susceptible individuals. VKH tends to affect the genetically predisposed, including Asians, Hispanics, and Middle Easterners.
The intraocular inflammation in VKH uveitis may be associated with serous retinal detachment, optic disk edema, vitritis, and, eventually, a “sunset glow” fundus, or one with a yellow-orange appearance due to depigmentation of the retinal pigment epithelium and choroid.
Initial treatment consists of corticosteroids followed by a transition to immunomodulatory drugs for long-term control. If VKH uveitis is treated promptly and aggressively, complications such as cataract, glaucoma, choroidal neovascularization, and subretinal fibrosis can be avoided, and patients can have a good outcome. However, until recently, little was known about whether initial therapy with a systemic corticosteroid plus an immunomodulatory drug could improve long-term visual outcomes in these patients.
To evaluate the effectiveness and safety of adding the organ-rejection immunosuppressant mycophenolate mofetil (CellCept/Roche) to a systemic corticosteroid to treat acute VKH uveitis at initial onset, Ahmed Abu El-Asrar, MD, and colleagues at King Saud University College of Medicine in Riyadh, Saudi Arabia, did a prospective study of 38 patients (76 eyes) with VKH uveitis.
Main outcome measures of the study were final visual acuity, degree of corticosteroid sparing, progression to chronic, recurrent granulomatous uveitis, and the development of complications, especially a “sunset glow” fundus. Mean follow-up was 37 ± 29 months (range, 9—120 mos).
Initial combination treatment achieved a visual acuity of 20/20 in 93% of the eyes studied. Moreover, corticosteroid sparing was achieved in all patients evaluated, and the mean interval between treatment initiation and tapering to ≤10 mg of corticosteroid daily was 4 ± 1 months (range, 3—7 mos).
Moreover, 22 patients, or 58%, discontinued treatment without a relapse of inflammation. Mean duration without treatment was 28 ± 20 months (range, 1—60 mos).
The Saudi team did not find progression to chronic recurrent granulomatous uveitis in any of the eyes studied. Ocular complications included glaucoma in two eyes (3%) and cataract in 5 eyes (7%). “Sunset glow” fundus did not develop in any of the eyes studied, and no systemic adverse events were associated with combination treatment.
As a result, the Saudi team concluded that initial treatment with systemic corticosteroids plus CellCept in patients with acute VKH uveitis prevented progression to chronic recurrent granulomatous inflammation and the development of a “sunset glow” fundus.
The study, “Mycophenolate mofetil combined with systemic corticosteroids prevents progression to chronic recurrent inflammation and development of ‘sunset glow fundus’ in initial-onset acute uveitis associated with Vogt—Koyanagi–Harada disease,” was published online in Acta Ophthalmologica on August 18, 2016.
Related Coverage:
Tocilizumab Effective for Uveitis in Juvenile Idiopathic Arthritis





