Article
Sedentary Time Increases Risk of Adverse Health Conditions
Author(s):
Vigorous physical activity may reduce the risk of non-communicable diseases, including rheumatoid arthritis and gout.
Sedentary time is associated with multiple adverse health conditions. Replacing vigorous physical activity (VPA), instead of moderate physical activity (MPA) and light physical activity (LPA), may reduce the risk of non-communicable diseases (NCDs), according to a study published in eClinical Medicine.1
“Sedentary time represents a major public health problem considering its high prevalence and health cost,” investigators stated. “In the UK, each adult spends an average 5 hours per day of sedentary activities, 30% adults are sedentary for at least 6 hours per day during the week, which rises to 37% on the weekend.”
Patients (N=360,047, aged 37-73 years) in the UK Biobank without 45 common NCDs were included in this prospective, population-based cohort study, conducted between April 2006 and December 2010. Self-reported information regarding sedentary time, including the amount of time spent watching tv, using a computer, and driving, as well as physical activity, measured by the International Physical Activity Questionnaire, were collected at baseline. A follow-up period analyzed diagnosis of common NCDs, according to the ICD-10 code, until 2020. Covariates included age, sex, ethnicity, employment status, socioeconomic status, alcohol intake, body mass index, and smoking status. Isotemporal substitution models determined differences in substituting sedentary time with LPA, MPA, and VPA, after adjusting for confounders.
The mean age of patients was 55.8 years and 54.5% were female. Patients who self-reported > 6 hours per day (n = 67034, 18.6%), compared with ≤ 2 hours per day sedentary time were more likely to have a higher risk for 12 of 45 NCDs (26.7%, P< 0.0011). According to a population attributable fraction (PAF) analysis for individual NCD significantly related to sedentary periods, 3.7%-22.1% of NCDs may not have occurred if sedentary time was reduced to less than 6 hours per day.
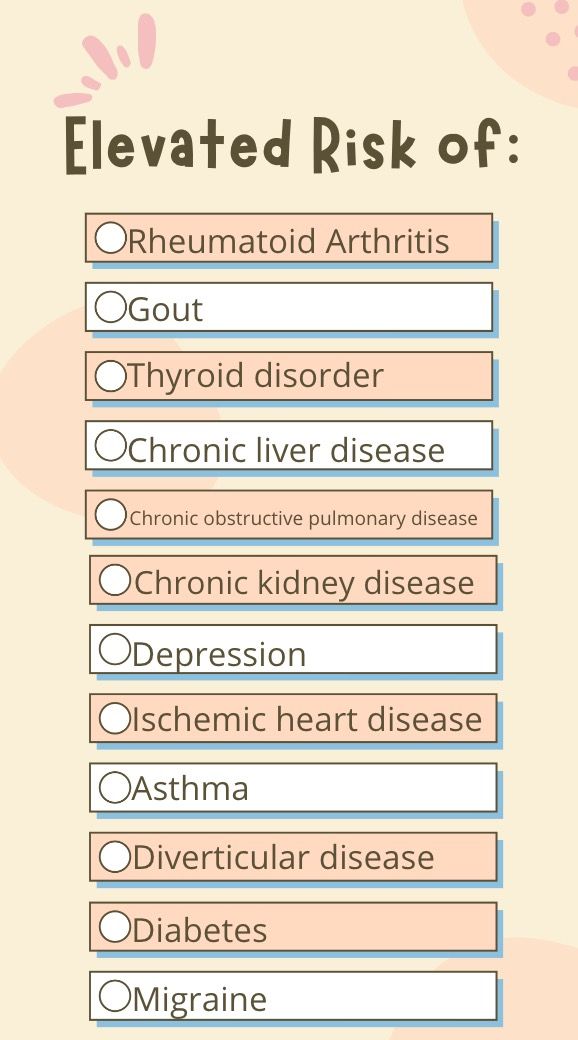
Replacing sedentary time with LPA, MPA, and VPA was associated with risk reduction 4, 6, and 10 types of NCDs, respectively. For patients with > 6 hours a day of sedentary time, replacing 1 hour a day with VPA was linked to a larger risk reduction (11%-31%) in diabetes, depression, diverticular disease, sleep disorder, and chronic liver disease.
The study was limited by its observational study design. Further, sedentary time and physical activity were subjectively measured, which may have introduced measurement bias. However, in recent years, the UK Biobank has implemented an objective measurement of activity levels via 7-day accelerometers in certain participants. Sedentary behavior was only evaluated by leisure time activities, such as watching television and computer time, without accounting for occupational sedentary behavior. Therefore, the sedentary time calculated in the study cannot be generalized to total sedentary time. Further research can be used to expand the current analyses. Diet was not included as a covariable, which may have influenced some NCDs. Lastly, results do not account for changes in sedentary habits at baseline and during the follow-up period.
“Our findings provide evidence on the detrimental effect of longer sedentary time,” investigators concluded. “Recommendations for sedentary time could indicate that any reduction in sedentary behavior coincides with increasing time spent in healthier alternatives to ensure positive replacement effects. Further studies are needed to investigate causality by an experimental intervention.”
Reference:
Cao Z, Xu C, Zhang P, Wang Y. Associations of sedentary time and physical activity with adverse health conditions: Outcome-wide analyses using isotemporal substitution model. EClinicalMedicine. 2022;48:101424. Published 2022 Apr 28. doi:10.1016/j.eclinm.2022.101424




