Article
Sports injuries in weekend warriors: 20 Clinical pearls
As a consequence of playing the role of the weekend warrior, recreational athletes often present with knee or leg pain. Generally, these patients can be categorized in 1 of 3 age-related groups (although, paradoxically, the injuries are not necessarily age-dependent):
As a consequence of playing the role of the weekend warrior, recreational athletes often present with knee or leg pain. Generally, these patients can be categorized in 1 of 3 age-related groups (although, paradoxically, the injuries are not necessarily age-dependent):
1. Young and aggressive. These patients tend to experience acute trauma, such as contusions, sprains (torn ligaments), and fractures, resulting from competitive sports activity. They also experience overuse injuries, which include various forms of tendinitis and stress fracture.
2. Middle-aged and "hanging on." Typically, patients in this group present with conditions resulting from overuse, such as bursitis, tendinitis, and stress fractures.
3. Older and arthritic. Most of these patients are out of shape and overweight and have elevated cholesterol levels and blood pressure. They are likely to have received an admonition from their physician to lose weight and to exercise, and they often exhibit symptoms resulting from overload of osteoarthritic joints.1
Most often, complaints from recreational athletes are minor injuries associated with overuse or lack of physical conditioning. However, the pain they experience can be a signal of a more ominous underlying condition. Therefore, the physician's task is to not only make the proper diagnosis and when the symptoms are minor, reassure the patient but also to treat the patient when the condition warrants and when the diagnosis is in doubt, pursue further workup.
In this article, I offer 20 "pearls," or practical pointers, geared to more effective diagnosis and management of the minor injuries that are common in recreational athletes (Table). These pearls are gathered from the literature, the counsel of mentors, and the experience gained during more than 30 years of professional practice in which I have frequently addressed the complaints and questions of weekend warriors experiencing pain.
1. Pain may signal a more harmful condition
"Doctor, I started to exercise on a treadmill and now my knee hurts. How do I know whether I should continue to exercise?"
This question, most often heard from older and arthritic patients, perhaps illustrates the most common reason why patients come to my office. Their knee pain may not be severe enough to force their exercise to a halt, but they are concerned that continued exercise may result in harm.
Patients can be reassured that the potential benefits of exercise far outweigh the discomfort they feel on initiating their conditioning program.2 However, their pain may be indicative of a harmful condition.
For example, the presence of a joint effusion should signal that more than simple overuse is involved and that activities consistently resulting in a swollen joint should be modified or abandoned. Pain that is accompanied by dramatic mechanical symptoms, such as painful locking or "giving way," should be investigated further to rule out an "internal derangement," such as loose bodies or torn menisci. The intensity and duration of pain are important factors-pain that progressively worsens with exercise and leads to a limp with daily activities should prompt modification or omission of the activity; pain that persists at rest and becomes severe at night requires further clinical investigation.
2. The heavy influence of excess body weight
"My knee hurts when I exercise and even when I walk up and down stairs. Please do something for me."
Many of the middle-aged recreational athletes with knee pain look for a passive means of relieving it-the pill, the brace, or even the operation that will "cure" their problem. They do not want to hear that their pain is exacerbated by their excess body weight or their weak and inadequate musculature or both.
My advice: resist the temptation to rid your office of these patients by giving them yet another NSAID or another brace. These are not solutions. Emphasize that the best solution for this problem is for the patient to take ownership of the treatment, which will include an active exercise protocol and a weight reduction program.3
3. Demonstrate that obesity is a big deal
"So I am a few pounds overweight. How can that be such a big deal for my knee pain?"
Consider that with activities of daily living and modest exercise, 2 to 6 lb of force are generated across the knee joint for every pound of a person's body weight.4 For some activities, forces across the patellofemoral joint can be as great as 20 times body weight.
In performing bending, kneeling, and climbing activities, for example, a 30-year-old woman with knee pain who weighed 120 lb at age 18 years, before her 3 pregnancies, and now weighs 285 lb is carrying an extra 165 lb of body weight. That can result in an additional 660 lb of force across the patellofemoral joint with each step. To convince patients that weight control is indeed an important factor in the management of knee pain, point out that obesity is the most common comorbidity of knee osteoarthritis in North American women.5,6 For this group of patients, performing aquatic exercises is a wonderful way to start an exercise program and avoid the depressing pain of a dry-land program.
4. Use the 10% rule
"I understand that I need to start exercising, and I joined a local health club. How can I avoid overuse injury?"
Recommend that when beginning an exercise program patients use the "10% rule": limit to no more than 10% per week any increase of intensity of exercise (eg, pace and distance for running or repetitions and resistance for weight training). Also, when organizing an exercise program, they should try to minimize the variables of change and avoid increasing distance, repetitions, and intensity at the same time.
Your patients should be reminded that they are making long-term commitments and even lifestyle changes. Entry into their program should have a low level of intensity that makes the entry as pleasant and pain-free as possible and the exercises comfortable and easy to perform. Suggest to patients that they pick a "slow friend" to begin the program with.
5. Organizing an appropriate fitness program
"How much exercise should I do?" Fitness (a level of cardiovascular efficiency judged to be physiological by available normative data) is and should be the goal for most patients, even recreational athletes. Fitness crosses over to training when athletes go beyond the amount of exercise required for cardiovascular efficiency alone and are conditioning their bodies for optimal performance of physical tasks.
Whether the patient is striving for fitness or training is a key factor to consider in determining how much exercise should be performed. Expectations for achieving fitness with exercise vary inversely with the patient's age-younger patients tend to have higher expectations than older patients. Each individual patient's current health and genetics are other influences.
Organization of an appropriate fitness program should involve consideration of all these factors. Such a program benefits from the collective input of the primary care physician for recognition of existing medical conditions and risk factors; a personal trainer; a cardiologist, when needed; and, ideally, an exercise physiologist.
6. Even weekend warriors can tear an ACL
"I was running for the ball while playing in an alumni game this past weekend and hurt my knee. What can you do for me?"
The patient went on to describe how another player cut in front of him when he was running. As he tried to avoid the other player, his knee seemed to go one way and his body another. He heard a "pop" in his knee and felt more pain than he had ever experienced. He could not continue to play, and the knee began to swell. This history depicts an acute tear of the anterior cruciate ligament (ACL), regardless of the patient's age, until proved otherwise.7
Management of an ACL injury involves several possible choices. The goal is to return the patient to a preinjury level of function. Although this may occur with nonoperative regimens of rehabilitation and bracing, the likelihood is much greater after surgical reconstruction. In particular, activities that involve hard running, pivoting, and jumping are better tolerated after reconstruction. The choices should be explained, and the patient should be given the opportunity to participate in the decision. If a patient is willing to modify his or her recreational involvement to emphasize low-risk activities, such as swimming and cycling, then he quite likely will do well without surgical intervention.
7. Acute patellar dislocation or subluxation?
"I was running and hurt my knee. My doctor says my knee is stable and I do not have a torn ACL."
Although an acute patellar dislocation or subluxation is less common than an ACL injury, it can have an identical clinical presentation. In the presence of normal radiographic findings and an examination that reveals good ligamentous stability, the "clue" that this knee injury may be related to an acute patellar subluxation or dislocation is the finding of localized tenderness in the region of the adductor tubercle and the medial femoral epicondyle. This region corresponds with the approximate site of attachment of the medial patellofemoral ligament, the primary static soft tissue stabilizer of the patella restricting lateral subluxation/dislocation. Although this ligament also can be torn from the medial border of the patella, the most frequent site of disruption is at the femoral attachment.
Apprehension with attempts at passive subluxation of the patella during the physical examination can also lead to the correct diagnosis. An MRI scan can reveal tears of the medial patellofemoral ligament, bone bruising of the lateral femoral condyle, and even osteochondral or chondral loose bodies, all directing us to the diagnosis of acute patellar dislocation.
8. Misinterpretation of knee injuries possible
"Could it be a different injury?" There are always opportunities for misinterpretation, and the history and physical findings for acute patellar subluxation or dislocation can be confused with those for other injuries. In the case described above, the tenderness over the medial femoral epicondyle is also close to the femoral attachment of the medial collateral ligament (MCL). A mechanism of injury that includes a valgus moment about the knee can be compatible with a patellar subluxation/dislocation as well as a sprain of the MCL. In an MCL sprain, however, the tenderness usually extends distally to varying degrees along the course of the MCL.
Stability testing may reveal increased valgus laxity. If needed, MRI will show edema and injury within the MCL. It is important to remember that multiple injuries can coexist. The finding of a torn MCL does not exclude the coexistence of an acute patellar dislocation and vice versa.
9. Acute knee effusions
"I hurt my knee playing in a volleyball league this weekend, and it is still swollen. This has never happened before."
Most injuries in recreational athletes are self-limited minor sprains or strains or mild overuse injuries. However, the patient who presents with a knee effusion is considered to have something wrong within the knee (intra-articular injury) until proved otherwise. Acute knee effusions most often are associated with torn menisci or ligaments, fractures, or articular cartilage damage.
10. Subtle symptoms may indicate a PCL injury
"I fell on my knee playing indoor soccer. I had Osgood-Schlatter disease as a teenager and have always had a bump on my tibia where the pain used to be. Now my knee is swollen, but I'm told it is only a bruise of my tibial tuberosity. Could something else be wrong?"
Again, swelling within the knee usually signals an intra-articular injury. In this case, the tibial tuberosity may be bruised, but the blow to the front of the tibia may have resulted in a posterior cruciate ligament (PCL) injury. In contrast to an ACL injury, in which the acute injury presents rather dramatically with severe immediate pain, a pop, and early swelling, the much less common PCL injury can result in subtle symptoms and clinical findings.
When a knee injury shows obvious evidence of a blow to the tibial tuberosity (especially if the knee was flexed at the time), always test for PCL insufficiency by performing the posterior drawer test. In this test, the patient is asked to lie supine on the examination table with knees flexed to 90°. The examiner sits on or otherwise stabilizes the foot of the leg being examined, grasps the leg just below the knee with both hands, and pushes the leg backward. If the tibia moves back under the femur, the PCL may be torn.
11. Lower leg pain: Shin splints and stress fractures
"My shins hurt. Is this a stress fracture?"
The term "shin splints" refers to pain in the legs that occurs with repetitive activity, most often running.8 The pain usually is located over the middle or distal third of the leg or both, along the posteromedial border of the tibia. Plain radiographs as well as other imaging studies, such as bone or MRI scans, may be needed to detect stress fractures.9 However, they can be suspected in the case of shin splints when the tenderness is localized to a small area of bone (a finger breadth or two) and the pain has progressed from only exercise-induced pain to pain with activities of daily living.10
12. Femoral stress fracture may lead to disability in runners
"I was training for the marathon and I got a severe pain in my thigh. It won't go away."
This pain should be a red flag for a femoral stress fracture until proved otherwise. Most stress fractures are simply a nuisance. A femoral neck stress fracture, if allowed to displace, may lead to lifelong disability resulting from osteonecrosis of the femoral head.11
This complication most often is avoidable if the fracture is recognized and managed early. The clue, in addition to the history, is the physical finding of anterior thigh or groin pain that is provoked by hip flexion or rotation during the examination. If plain radiography results are normal (as they often are), a bone scan or, preferably, an MRI is required to rule out this potentially serious condition.
13. Tennis leg or acute Achilles tendon rupture?
"I was playing tennis last night and my leg gave way. It felt like someone kicked me in the back of my calf."
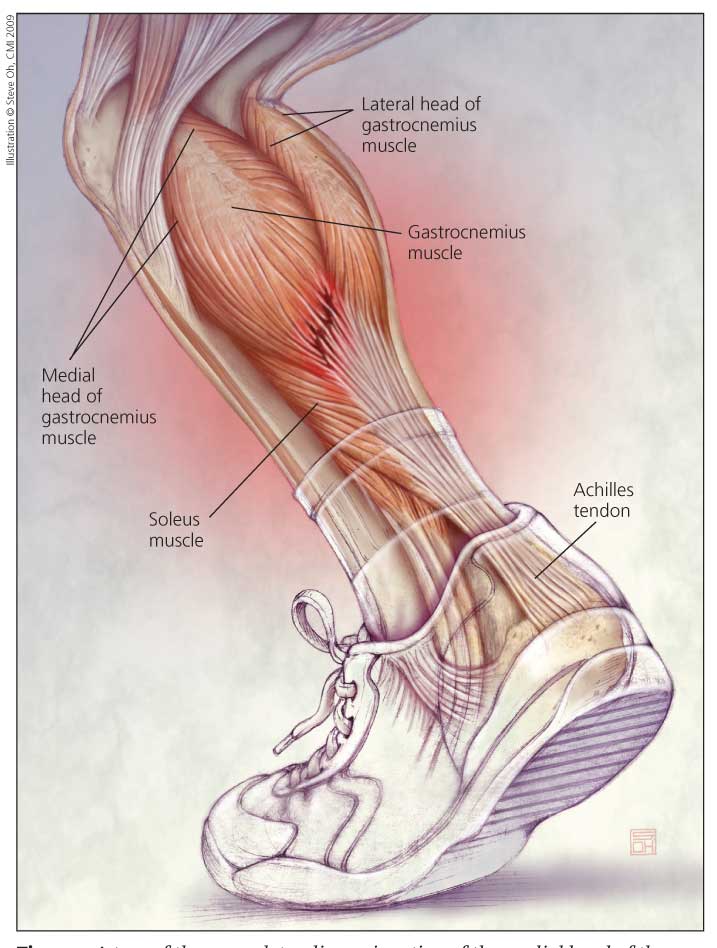
Figure – A tear of the musculotendinous junction of the medial head of the gastrocnemius muscle is known as tennis leg because this injury, common in recreational athletes, most often occurs in tennis players. The injury results from an acute forceful push-off with the foot and often occurs during a lunging shot when maximum tension is placed on the gastrocnemius as the lengthened muscle is contracted. Tearing also may occur in the soleus muscle. Tennis leg can be differentiated from an acute rupture of the Achilles tendon by noting the location of tenderness.
This common history is nearly pathognomonic of injury in the gastrocnemius-soleus muscle-tendon unit. A tear of the musculotendinous junction of the medial head of the gastrocnemius that results from an acute forceful push-off with the foot is known as tennis leg, because it occurs frequently in tennis players (Figure).12 One common mechanism of injury occurs during a lunging shot. The knee on the player's back leg is extended while the foot is dorsiflexed; maximum tension is placed on the gastrocnemius as the lengthened muscle is contracted at the push-off.
Tennis leg can be differentiated from an acute rupture of the Achilles tendon by noting the location of tenderness. In the former, tenderness is posteromedial at mid-calf; in the latter, tenderness is 1 to 6 cm proximal to the calcaneus over the Achilles tendon.
Also use the Thompson test. Ask the patient to lie prone on the examination table with his feet hanging off the end. A gentle squeeze of the calf elicits plantar flexion of the foot. If this squeeze does not elicit an amount of plantar flexion identical with that of the noninjured leg, the test result is considered abnormal and consistent with an acute rupture of the Achilles tendon.
14. Occult fractures with ankle sprains
"I sprained my ankle 6 weeks ago. It still hurts and gives way."
Most common ankle sprains are self-limited and are not reported. In some studies of ankle sprains, however, a significant incidence of occult associated fractures has been demonstrated.13 Most often, these are chip fractures of the talus.
Because the fractures that involve the talar dome are intra-articular injuries, they can be problematic. Even if the initial radiography results are interpreted as normal, it is worthwhile to repeat the x-ray films at a later time to rule out an occult fracture. If the symptoms and history warrant, CT or MRI scanning can be helpful in detecting these elusive fractures.
15. Restore strength and proprioception
"I sprained my ankle 8 weeks ago, and my x-ray and CT scan results are normal, but my ankle still hurts and gives way. What is going on?"
This scenario usually is reflective of incomplete or inadequate rehabilitation. Ankle injuries can lead to a period of relative weakness of the surrounding musculature (possibly because of altered activity, immobilization, or reflex inhibition with pain and swelling) and diminished proprioception skills.
16. Plantar fasciitis: Common, persistent, and troublesome
"My heel hurts. My doctor found a 'spur.'"
The spur seen on the plantar aspect of the calcaneal tuberosity is not the problem but rather a result of underlying inflammation in the plantar fascia attachment site. Most patients with plantar fasciitis should be treated using a nonoperative approach.14
17. Nighttime splinting in dorsiflexion for plantar fasciitis
A useful adjunct to treatment may be nighttime splinting in dorsiflexion. Most persons sleep with their feet plantar flexed; the plantar fascia is most relaxed in this position and receives "healing time." With the first weight bearing in the morning, however, this healing is immediately interrupted and typically pain is experienced as the fascia is suddenly stretched. In theory, nighttime splinting allows the healing time to take place with the fascia under tension so that the first weight bearing in the morning does not result in reinjury.
18. Toe banging, blisters, and black toe
"I have been running for years without toe problems. This past season I had blisters and black toenails after long runs or races. What can I do?"
It is often assumed that feet do not "grow" after skeletal maturity, but shoe size does change as persons age. Gradual stretching of plantar fascial support leads to loss of the longitudinal arch and a relative lengthening of the foot. Advise patients to buy a pair of shoes a size larger to provide needed room in the toe box to avoid toe banging and the blisters and black toe that often result from it.
19. Fluid replacement in marathon running
"I'm training for my first marathon and someone told me it is possible to drink too much water. Is that true and, if so, how much fluid replacement is enough?"
Drinking too much water, even sports drinks, can result in hyponatremia-a potentially life-threatening condition involving a deficiency of salt as well as an overload of water-in even the most experienced athletes. The risk of hyponatremia is proportional to the extent of time involved in extreme exertion; it is a significant risk in running marathons and, especially, ultramarathons.
Traditionally, drinking large amounts of water or sports drinks prophylactically (the "you can't drink too much" theory) has held favor. The current wisdom calls for a "drink when you are thirsty" recommendation to help avoid the possibility of fluid overload and hyponatremia.
20. Bloody nipples in long-distance runners
"I just completed my first marathon. My nipples hurt and there was blood in my shirt in the area around them. How can I prevent it?"
Bloody nipples is a common condition in men after long runs on hot days that can be very painful, especially the day after the run. Shirt abrasion resulting from the several thousand "bounces" during running rubs the nipples raw, even when the runner is wearing a lightweight running shirt.
To prevent bloody nipples, advise patients to avoid wearing a running shirt that has lettering or pictures embossed over the breast area. They should apply adhesive bandages or a lubricant over the nipples before an extended run to provide a protective coating.
References:
References1. Vad V, Hong HM, Zazzali M, et al. Exercise recommendations in athletes with early osteoarthritis of the knee. Sports Med. 2002;32:729-739.
2. Galloway MT, Jokl P. Aging successfully: the importance of physical activity in maintaining health and function. J Am Acad Orthop Surg. 2000;8:37-44.
3. Jakicic JM, Marcus BH, Gallagher KI, et al. Effect of exercise duration and intensity on weight loss in overweight, sedentary women: a randomized trial. JAMA. 2003;290:1323-1330.
4. Huberti HH, Hayes WC. Patellofemoral contact pressures: the influence of q-angle and tendofemoral contact. J Bone Joint Surg. 1984;66A:715-724.
5. Hart DJ, Doyle DV, Spector TD. Incidence and risk factors for radiographic knee osteoarthritis in middle-aged women: the Chingford Study. Arthritis Rheum. 1999;42:17-24.
6. Felson DT, Anderson JJ, Naimark A, et al. Obesity and knee osteoarthritis. The Framingham Study. Ann Intern Med. 1988;109:18-24.
7. James SL. Running injuries to the knee. J Am Acad Orthop Surg. 1995;3:309-318.
8. Thacker SB, Gilchrist J, Stroup DF, Kimsey CD. The prevention of shin splints in sports: a systematic review of literature. Med Sci Sports Exerc. 2002;34:32-40.
9. Brukner P. Exercise-related lower leg pain: bone. Med Sci Sports Exerc. 2000;32(3 suppl):S15-S26.
10. Perron AD, Brady WJ, Keats TA. Principles of stress fracture management: the whys and hows of an increasingly common injury. Postgrad Med. 2001;110:115-118, 123-124.
11. Shin AY, Gillingham BL. Fatigue fractures of the femoral neck in athletes. J Am Acad Orthop Surg. 1997;5:293-302.
12. Millar AP. Strains of the posterior calf musculature (“tennis leg”). Am J Sports Med. 1979;7:172-174.
13. Renstrom PA. Persistently painful sprained ankle. J Am Acad Orthop Surg. 1994;2:270-280.
14. Gill LH. Plantar fasciitis: diagnosis and conservative management. J Am Acad Orthop Surg. 1997;5:109-117.




