News
Article
Study Details Ocular Repercussions, Structural Changes After COVID-19 Infection
Author(s):
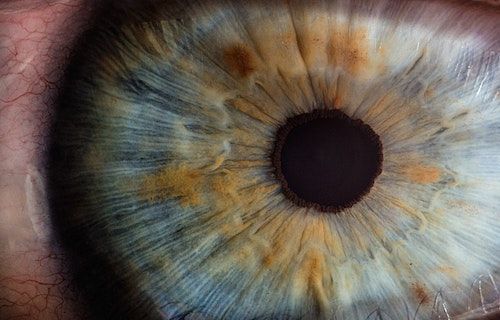
Investigators observed differences in choroidal and inner neural layers among patients previously infected with COVID-19 compared to healthy controls.
Credit: Unsplash
Findings from a recent cross-sectional study are providing clinicians with an overview of neurodegenerative and vascular modifications of the retina among patients who have recovered from COVID-19.
Ophthalmologic characterization showed a non-glaucomatous neuropathy trend pattern among patients previously infected with COVID-19, further calling attention to an increase in choroidal thickness as a result of vascular changes among these patients compared to healthy controls.1
“Neurotropic capabilities of SARS-COVs allow viruses to reach the central nervous system by hematogenous neuronal dissemination. The human retina, as an extension of the Central Nervous System, may have some neurodegenerative and/or vascular modifications related to COVID-19,” wrote Ilda Maria Poças, of Lisbon School of Health Technology in Portugal, and colleagues.1
An infectious disease caused by the SARS-CoV-2 virus, COVID-19 is highly contagious and can lead to severe illness. According to the World Health Organization (WHO), more than 760 million cases and 6.9 million deaths have been recorded worldwide since December 2019, although the actual number is thought to be higher. Typically, infection with the virus is associated with fever, chills, and a sore throat, which the WHO recognizes as the most common symptoms of COVID-19.2
Beyond its usual respiratory impacts, ocular manifestations of COVID-19 present another complication of the disease, with a growing number of reports prompting investigations into ocular signs, symptoms, and transmission. Early studies postulated ocular symptoms of COVID-19 were rare, although further research has alluded to lasting ocular repercussions among those who were previously infected and have since recovered.3
Investigators sought to compare ophthalmologic characteristics including choroidal and inner neural layers among patients previously recovered from COVID-19 and healthy controls. Neurodegenerative and vascular histological assessments were performed using spectral-domain optical coherence tomography and the mean thickness was measured in Early Treatment Diabetic Retinopathy Study (ETDRS) subfields. Investigators further obtained retinal nerve fiber layer, Ganglion cell layer, and subfoveal choroidal thickness through semi-automatic measurement.1
In total, 96 participants were included in the study, including 56 previously infected with COVID-19 and 40 healthy controls. Investigators observed significant differences in retinal thickness across nearly all inner ETDRS subfields, including nasal 3 mm (P = .025), I3 (P = .049), and temporal 3 mm (P = .009). Decreases in neural layers were found in the nasal 3 mm (P = .049) and temporal 3 mm (P = .029) were also observed during ganglion cell layer assessment.1
Among patients in the COVID-19 group, the peripapillary retinal nerve fiber layer thickness was thinner in superior temporal (P = .019), nasal (P = .002), inferior temporal (P = .046) and global (p = .014) compared to the control group. Investigators also pointed out an increase in the subfoveal choroidal measurement in the COVID-19 group (P = .002).1
“Participants who had recovered from COVID-19 showed a non-glaucomatous neuropathy trend pattern. We found differences closer to the classic description of the ‘bow-tie’ observed in other neurological as compressive neuropathies at the chiasma location. OCT assessment also showed an increase in choroidal thickness as a result of vascular changes,” investigators concluded.1
References:
- Poças IM, Lino P, Silva C, et al. Ocular repercussions in COVID-19 patients: structural changes of the retina and choroid. Strabismus. https://doi.org/10.1080/09273972.2023.2278639.
- World Health Organization. Coronavirus disease (COVID-19). Newsroom. August 9, 2023. Accessed December 6, 2023. https://www.who.int/news-room/fact-sheets/detail/coronavirus-disease-(covid-19)
- Hu K, Patel J, Swiston C, et al. Ophthalmic Manifestations of Coronavirus (COVID-19). Statpearls. May 24, 2022. Accessed December 6, 2023. https://www.ncbi.nlm.nih.gov/books/NBK556093/





