Article
Study Shows Intravitreal Methotrexate Injection Is Effective in Patients with Diabetic Macular Edema Who Do Not Respond to Intravitreal Bevacizumab
Author(s):
Intraocular injections of methotrexate have been used successfully to treat indeterminate and sarcoid uveitis as well as age-related macular degeneration. Methotrexate injection’s record of success in treating these inflammatory eye diseases prompted researchers to evaluate its efficacy in treating persistent diabetic macular edema.
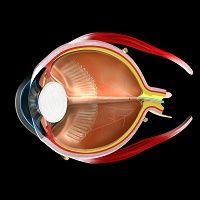
Despite multiple intravitreal injections of anti-vascular endothelial growth factor (VEGF) agents, diabetic macular edema (DME) may persist in a substantial number of patients. Inflammation is an important contributor to diabetic retinopathy, and intraocular levels of inflammatory cytokines and chemokines are elevated in patients with DME.
Intraocular injections of the anti-inflammatory, anti-neoplastic agent methotrexate have been used successfully to treat indeterminate and sarcoid uveitis as well as age-related macular degeneration.
Methotrexate injection’s record of success in treating these inflammatory eye diseases prompted an Iranian team to evaluate its efficacy in treating persistent DME in a prospective interventional case series recently reported in Graefe’s Archives for Clinical and Experimental Ophthalmology.
The study included 16 patients (18 eyes) with persistent DME affecting the fovea. DME was defined as persistent if it remained unresponsive to at least three consecutive injections of bevacizumab or two consecutive injections of bevacizumab plus macular photocoagulation.
All eyes found to have persistent DME at the Iran University Eye Research Center from September 2013 to January 2015 were included in the study. Main outcome measures were central subfield thickness (CST) and maximum retinal thickness (MRT). Secondary outcome measure was best-corrected visual acuity (BCVA).
The investigators gave each eye a 0.16-mL (400-μg) intravitreal injection of methotrexate (Haupt Pharma) then measured BCVA with a Snellen chart and CST and MRT with spectral-domain optical coherence tomography 6 months after methotrexate injection. By the end of the study, improvement in BCVA of at least two lines was found in three eyes (16.6%), and no eye lost visual acuity.
After 6 months of follow-up, CST decreased in seven eyes (38.8%) but increased more than 10% from baseline in five eyes (27.7%). There were no major complications (eg, endopthalmitis or retinal detachment).
Based on these results, the investigators concluded that intravitreal methotrexate injection is effective in treating persistent DME is a subset of eyes.
However, they acknowledged that larger studies are needed to confirm their findings in this small sample of patients. They also noted that repeated intravitreal injections of methotrexate may be useful in eyes with an initial response to therapy.
According to the Iranian team, their results suggest that intravitreal methotrexate may also have a role in treating naïve eyes with DME in patients with systemic factors that contraindicate the use of anti-VEGF agents or in those who are unable to afford or are unwilling to pay for these expensive agents. They also noted that methotrexate could be used with anti-VEGF agents to enhance their therapeutic effect.