Article
Survey Addresses Concerns Regarding Reproductive Healthcare Communication in Women with RA, PsA
Author(s):
Although the proportion of women treated with biologics continues to grow, data on treatment recommendations among both physicians and female patients of childbearing age remain limited.
Holistic, collaborative, multidisciplinary, and integrated communication between physicians and women of childbearing age is lacking, according to a study published in Springer.1 Medical treatment and family planning, particularly among women of childbearing age with rheumatoid arthritis (RA) and psoriatic arthritis (PsA), should be considered within this patient population. Patient-centered care including reproductive choices should be integrated as a part of routine clinical practice.
“The proportion of women being treated with biologics is growing,” investigators explained. “However, data on treatment recommendation awareness among treating physicians and women who are considering pregnancy and family planning are limited.”
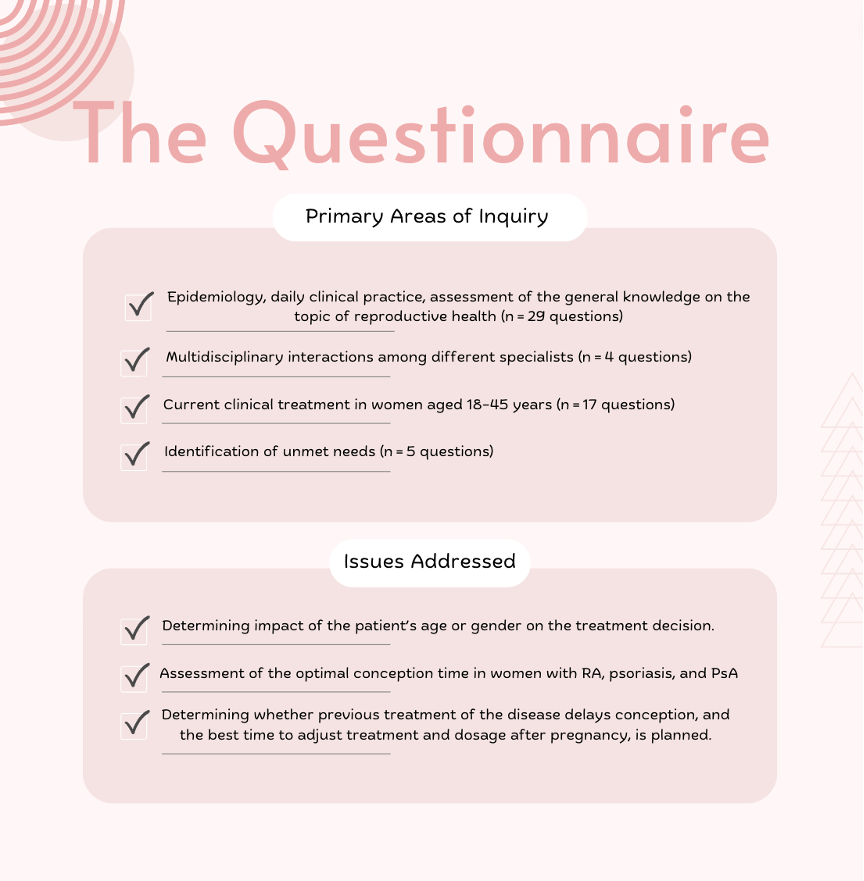
An English-language, 55-question survey was developed to identify the current practices of physicians regarding the reproductive health needs of women with RA, PsA, and psoriasis in the Czech Republic, Slovakia, and Hungary. The questionnaire was designed to simultaneously elicit spontaneity of physicians while allowing for the processing of responses, mutual comparison, and overall assessment. The survey obtained information from 120 physicians, including 82 rheumatologists and 38 dermatologists.
Female patients of reproductive age (aged 18 to 45 years) with moderate-to-severe disease encompassed 10-30% of all respondents. Roughly two-thirds of physicians discussed family planning with their patients when making the diagnosis. Rheumatologists collaborated with other specialists more frequently when compared with dermatologists and gynecologist/obstetricians. Pregnancy effects were the top concern for female patients.
Approximately half of the rheumatologists revised treatment 6 months prior to when the patient planned on becoming pregnant (44% [n = 36/81]). However, dermatologists acted much sooner (26% [n = 10/38]), acting 2 to 3 years prior planned parenthood. While rheumatologists selected systemic glucocorticoids as firs-line treatment to counteract pregnancy flares, dermatologists preferred topical corticosteroids.
Although gender alone did not influence treatment choice in 11% of dermatologists and 39% of rheumatologists, all dermatologists and 96% of rheumatologists were influenced by the patient’s fertility and pregnancy. Disease severity and uncontrolled disease were the main risk factors linked to conception in this patient population. In fact, 53% of dermatologists and 79% of rheumatologists believed that poor disease control was associated with poor pregnancy outcomes. Of the most valuable sources of information as determined by physicians, congresses and interdisciplinary forums were the most highly rated. Patient education and collaboration were noted as key factors in reducing unplanned pregnancies.
A cross-border investigation, from the perspective of both rheumatologist and dermatologist, strengthened the study. However, investigators did not evaluate or categorize the individual physicians’ level of experience with biologics or reproductive health and instead based data on actual clinic experience. Investigators theorize that those who have had more exposure to this approach would be more willing to utilize it. The lack of formal survey validation, and the fact that the survey was provided in English, further limits the study.
“To improve the reproductive health of sexually active women of childbearing age in Central Europe who have chronic inflammatory diseases (CID), rheumatologists and dermatologists must improve their education and work with other specialists,” investigators concluded. “More timely discussions with women of reproductive age and family planning are needed to educate them about the disease's effects on their childbearing potential and the selection of treatment options based on their reproductive goals. Best practices in patient-centered care must consider each patient's reproductive decisions in their treatment planning to give the best patient-centered care.”
Reference:
Olejárová M, Macejová Ž, Gkalpakiotis S, Procházková L, Tóth Z, Prágr P. Reproductive Healthcare in Women with Rheumatoid Arthritis and Psoriatic Diseases in Routine Clinical Practice: Survey Results of Rheumatologists and Dermatologists [published online ahead of print, 2022 Sep 24]. Rheumatol Ther. 2022;10.1007/s40744-022-00488-z. doi:10.1007/s40744-022-00488-z




