Article
The Role of the Skin Microbiome in Health and Disease
Author(s):
The skin microbiome may have beneficial influence on the skin through three mechanisms: direct inhibition of pathogen growth, improvement of the host's immune system, and education and priming of the adaptive immune system
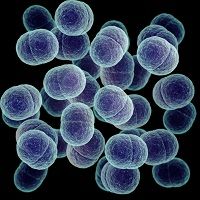
The diversity of microbial species on the human skin is daunting, and a few hundred species have been identified on it. It is estimated that the human body is composed of 10% of human cells and 90% of bacteria. Human skin cells are outnumbered 33 to 1. To discuss the interaction between the human skin and the bacterial environment surrounding it, Richard L. Gallo, MD, PhD, Professor of Medicine and Pediatrics, and Chief of the Division of Dermatology at the University of California, San Diego, gave a talk at the American Academy of Allergy, Asthma and Immunology’s 2015 annual conference in Houston, TX.
The interactions between bacteria and the human skin may be detrimental or beneficial. In this lecture, Gallo concentrated on the beneficial interactions, which are most probably mutualistic (ie, both host and bacteria benefit from the interaction). He speculated that the role of the immune system in this relationship is to maintain the mutualistic interaction.
His laboratory was one of the first to identify antimicrobial peptides (AMPs), which are produced by the host’s epithelial cells and are important in the defense mechanisms of the skin. He told the audience that decreased expression of AMPs in mice, animal models, and humans is linked to the development of atopic dermatitis. In this disease, the production of a few of the most potent AMPs is severely impaired. He hypothesized that the skin microbiome affects the epidermal defense systems and the host’s immune system, which in turn alters the skin microbiome, generating a constant cycle.
According to Gallo, the skin microbiome may have beneficial influence on the skin through three mechanisms: direct inhibition of pathogen growth, improvement of the host’s immune system, and education and priming of the adaptive immune system. Indeed, germ-free mice have defective education and priming of the immune system.
Gallo has previously demonstrated that S. epidermidis, which is normally present in the human skin, produces two types of AMPs. To evaluate the effect of these AMPs on inflammation, mice have been injected with poly I:C extracts (a pro-inflammatory agent) obtained from S. epidermidis and vehicle. Mice treated with poly I:C and S. epidermidis extracts did not develop a robust inflammatory response such as that observed in mice treated with poly I:C only. He concluded that S. epidermidis protected the host against inflammation.
In order to identify the localization of bacteria in the skin, studies have been performed in normal health skin. Bacteria have been identified mostly in hair follicles. Lower amounts of bacteria have also been identified in the dermis and the dermal adipose tissue. Gallo speculated that this distribution of bacteria might represent a filter thatwould distribute external microorganisms within the different strata of the skin to preserve a healthy environment.Additionally, he has shown that disruption of the dermal adipose layer is linked to the colonization of the skin by S. aureus, a phenomenon commonly observed in patients with atopic dermatitis.
Finally, Gallo showed some promising evidence that manipulation of the microbiome in a human subject heavily colonized with S. aureus improved atopic dermatitis.
In conclusion, the microbiome is an important component of the host’s immune system. The appropriate relationship between the microbiome, the host and the environment seems to be a key factor for the equilibrium and health of the skin.




