Article
Transforaminal Morphine Effective for Lumbar Radicular Pain, But Not Superior to Tramadol Injection
Author(s):
Transforaminal epidural steroid injections (TFEI) have become a more common approach to relieving chronic lumbar radicular pain, but until now, no published clinical reports had directly compared morphine with tramadol for that indication.
Transforaminal epidural steroid injections (TFEI) have become a more common approach to relieving chronic lumbar radicular pain, which “radiates” along the sciatic nerve, most commonly as a result of a herniated spinal disc. However, no published clinical reports had directly compared morphine with tramadol for that indication — or even addressed the efficacy of morphine via TFEI in radicular pain — until an analysis of the treatments was published in the July 2013 edition of the Korean Journal of Pain.
For the “Comparison of Morphine and Tramadol in Transforaminal Epidural Injections for Lumbar Radicular Pain” study, Chan Hong Park, MD, from the Department of Anesthesiology and Pain Medicine at Daegu Wooridul Spine Hospital in Korea, randomized 59 patients diagnosed with the chronic neuropathic pain condition, also known as sciatica, to receive either TFEI of 0.2 percent ropivacaine in combination with 2.5 milligrams of morphine sulfate, or TFEI of 25 milligrams of tramadol — which is trademarked as Ultram, Ultracet, Ryzolt, and ConZip in the US — plus normal saline.
During the first two weeks after the injections, all patients received non-steroidal anti-inflammatory drugs and muscle relaxants, though the patients who were unresponsive to those medications were provided opioid or non-opioid analgesics after their first follow-up visit.
According to Park, results at two weeks after TFEI and final results at three months post-treatment showed both groups had significantly lower mean pain scores from baseline measures, thus establishing the efficacy of morphine via TFEI in sciatica, but also rejecting transforaminal tramadol’s superiority to transforaminal morphine — and vice versa — in treating the chronic nerve pain condition. However, Park noted that the “patients given morphine did trend toward greater radicular pain reduction … albeit not statistically significant.” (Table)
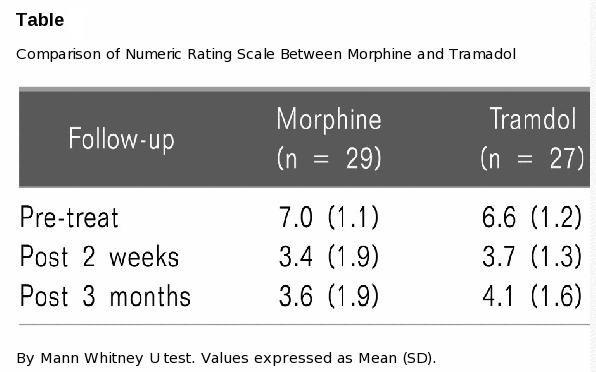
But the limitations of the study may have impacted that finding, as Park acknowledged that the “injectate volumes were not uniform” and “patients were not differentiated by nature of pain, (such as) neurogenic claudication or resting, spontaneous pain.” Even if TFEI morphine was shown to be statistically superior to TFEI tramadol for lumbar radicular pain, Park noted that “incidences of allergic rash, itching, sedation, and respiratory depression and sedation score were higher in the morphine group” and “further study is needed to determine the optimum morphine dosage under these circumstances.”
“Although local anesthetic and corticosteroid combination is typically used for TFEI of the lumbar spine, the choice of drugs used for this kind of intervention remains controversial,” Park concluded. Nevertheless, the current study proved “TFEI of an opioid plus local anesthetic to be effective in treating radicular pain.”





