Article
USPSTF Reaffirms Endorsement for Statin Use in Primary Prevention Settings
The US Preventive Services Task Force (USPSTF) has released a new recommendation statement outlining the group’s stance related to the use of statin therapy for the primary prevention of cardiovascular disease in adult patients.
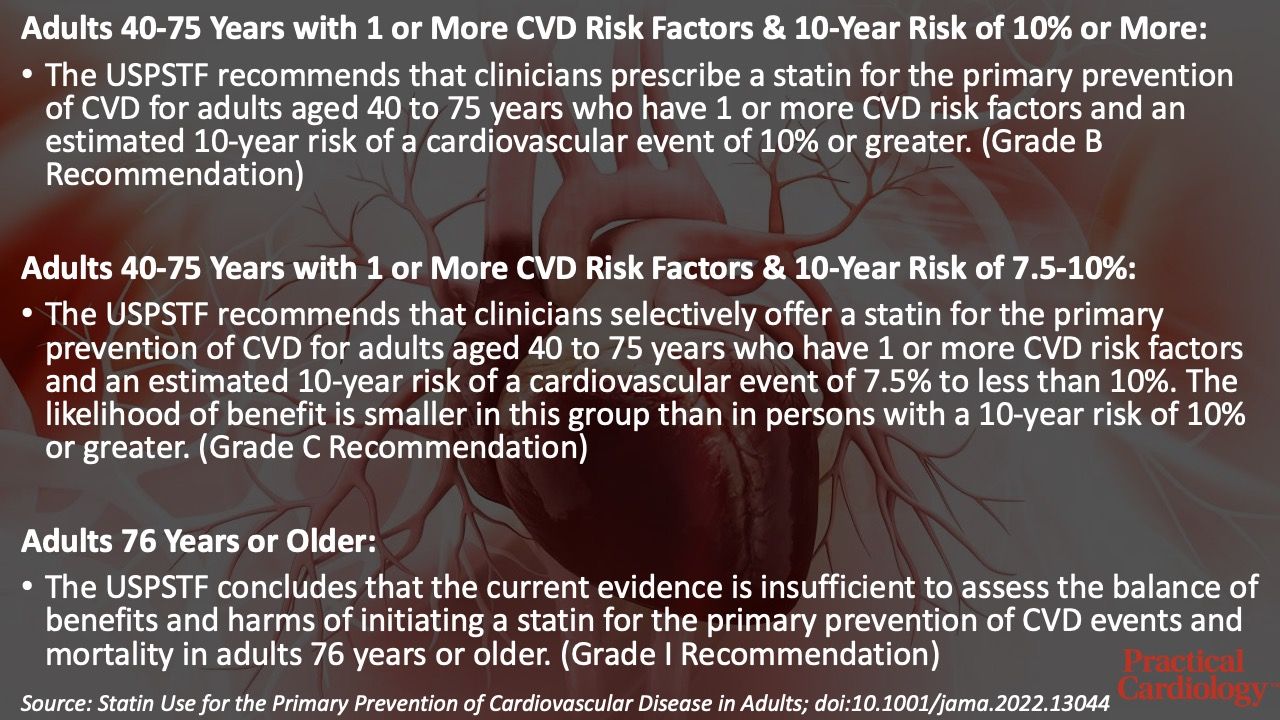
Released on August 23, the 8-page recommendation statement, which serves as an update to the group’s 2016 recommendation statement on the topic, recommends statin use for the primary prevention of cardiovascular disease among adults aged 40-75 years who have 1 or more cardiovascular risk factors and an estimated 10-year CVD risk of 10% or greater while recommending selective offering of statin therapy for the primary prevention among adults aged 40-75 years with 1 or more risk factors and an estimated 10-year risk of 7.5% to less than 10%.
“Importantly, we are using this final recommendation statement to call attention to inequities in the rates of CVD and in access to and use of statins,” says Task Force member Katrina Donahue, MD, MPH, in a statement from the USPSTF. “It is essential that we work to better understand the causes of these inequities and reverse the negative impacts of systemic racism on cardiovascular health.”
Summary of USPSTF Recommendations on Statins for Primary Prevention
The recommendations made within the statement are based on a systematic review of data from the Ovid MEDLINE, Cochrane Central Register of Controlled Trials, and Cochrane Database of Systematic Reviews detailed in an evidence report published in JAMA. This review included 26 studies, with 22 randomized controlled trials with 6 months to 6 years of follow-up comparing statins against placebo or no statin, 1 trial comparing statin intensities, and 3 observational studies reporting harms of statin use.
In this review, results suggested statins were significantly associated with decreased risk of all-cause mortality (RR, 0.92 [95% CI, 0.87 to 0.98]; ARD, −0.35% [95% CI, −0.57 to −0.14%]), stroke (RR, 0.78 [95% CI, 0.68 to 0.90]; ARD, −0.39% [95% CI, −0.54 to −0.25%]), myocardial infarction (RR, 0.67 [95% CI, 0.60 to 0.75]; ARD, −0.85% [95% CI, −1.22% to −0.47%]), and composite cardiovascular outcomes (RR, 0.72 [95% CI, 0.64 to 0.81]; ARD, −1.28% [95% CI, −1.61 to −0.95%]), but the association with cardiovascular mortality was not statistically significant (RR, 0.91 [95% CI, 0.81 to 1.02]; ARD, −0.13%). When assessing the benefits vs harms of statin therapy, results indicated statin therapy was not significantly associated with an increased risk of serious adverse events (RR, 0.97 [95% CI, 0.93 to 1.01]), myalgias (RR, 0.98 [95% CI, 0.86 to 1.11]), elevated alanine aminotransferase level (RR, 0.94 [95% CI, 0.78 to 1.13]), or increased diabetes risk overall (RR, 1.04 [95% CI, 0.92 to 1.19]).
Investigators pointed out a single trial found high-intensity statin therapy was significantly associated with increased risk, but there were no clear differences in outcomes based on statin therapy outside of this instance. Later in their evidence report, the authors noted benefits observed in the review were consistent across patient subgroups, but data for patients older than 75 years was sparse.
In an editorial published in JAMA Cardiology, Neil Stone, MD, and Philip Greenland, MD, along with Scott Grundy, MD, PhD, compare the recommendations made by the USPSTF to other guidelines and recommendations from other international bodies.
“In summary, the new USPSTF recommendations for statin therapy agree with current AHA/ACC/MS guidelines that patients aged 40 to 75 years with a high enough 10-year ASCVD risk merit statin therapy,” wrote the trio. “There is disagreement on the recommended thresholds for statin initiation and how the clinician and patient resolve the frequent situation in which a risk estimation makes treatment decisions uncertain.”
This study, “Statin Use for the Primary Prevention of Cardiovascular Disease in Adults,” was published in JAMA.





