Article
Vegan Diet: It's Powerful Medicine Kim Williams, MD, says in Q&A
Author(s):
The American College of Cardiology's outgoing President Kim A. Williams, MD, went vegan in 2003 and never looked back. He talks about the diet's power to heal and how being the ACC's first vegan leader played out.
Editor’s Note: Outgoing American College of Cardiology President Kim A. Williams, MD, went vegan in 2003. He reduced his LDL cholesterol dramatically. MD Magazine contributor, Megan Daily, interviewed him about his healthy lifestyle and how his advocacy of a plant-based diet for heart health goes over with colleagues in a specialty where drugs and interventions play such a big role.
Q: What it is like standing in front of a room full of cardiologists and saying you want them to put themselves out of business?
And, I didn’t get booed off the stage—that was wonderful, and I can say it parallels the reaction of the entire ACC.
Q: You mean your vegan message has played well with your colleagues?
I haven’t gotten negative feedback. Even when they eat meat or don’t exercise, my colleagues don’t feel insulted because they know this [vegan diet] is the best thing to do for the population.
Q: Isn't eating meat a big part of American culture, like BBQ on the Fourth of July?
It is. But getting into the science of plant-based nutrition is interesting. Barbecue isn’t a bad thing as long as it’s a plant. All those carcinogenic things that happen when you char meat, they don’t apply to charred popcorn and things like that.
Q: So it's not the grilling process that makes food unhealthy?
You may think it’s got to be really dangerous, but it turns out it’s not. That’s a good example of how the science not only needs to be updated, it has to be disseminated—having great mortality data in the American Journal of Clinical Nutrition is wonderful but it doesn’t help if that’s not on your reading list. We need to get the word out more and more.
Q: You mean like the findings in the INTERMAP study in 2006 that showed the inverse relationship between blood pressure and intake of vegetable protein?
Absolutely.One of the more dangerous things about the vegan diet--and it's happened to me--is that I encourage a patient with high blood pressure to adopt a vegetarian diet and they do, but they forget their home blood-pressure monitoring.
Next thing you know they are in some emergency room with a [very low] blood pressure of 80 over 50 because they are still taking medication that I gave them for a disease they don't have anymore.
Q: The diet works that well?
It’s very powerful. If people just understood how you could make hypertension just disappear in weeks to months by changing the diet, in a large number of people, they’d find it pretty amazing.
Q: So, what is the obstacle? Is it culture? Is it that the data in the studies are not convincing?
There is a little bit of variability in the data. But there is a recently published analysis by [Yoko] Yokoyama that looked at 32 studies. Three of them said a vegan diet can raise blood pressure, but the majority showed a significant improvement. When you add them all up the data are positive. Obviously there are other things—drinking to excess, not exercising—which can raise blood pressure despite a vegan diet. It has to be part of a healthy approach to living.
Q: Do physicians have to be practicing what they preach to get the message to their patients?
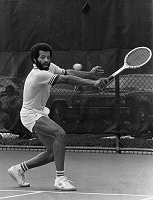
It’s very difficult to be told by someone who is overweight that you need to lose weight. We do need to model good behaviors. (Photo, right, Williams as captain of the U.Chicago tennis team)
Q: You’ve talked a lot about how your personal history convinced you to change to a vegan diet. Is that the motivator for most cardiologists who suggest a meat-free diet to patients?
That’s growing more common, but if you google “vegan cardiology” you will see some strange things. I saw one that said “I had a patient with lupus myocarditis and they went vegan and everything went normal,’, so sometimes it’s not personal, it’s clinical experience that makes them change.
Q: You’re saying these stories about vegan diets curing other ailments are mostly true?
Oh, yes. There are a variety of diseases that have been either cured, or dramatically improved, there’s data on multiple sclerosis, rheumatoid arthritis, lupus, and it would be nice if there were large randomized trials.
Q: There haven’t been many?
The last vegan diet trial that I looked up was about ulcerative colitis. I was blown away by the data. I had heard about Dr. Dean Ornish’s study long ago, on prostate cancer and that a vegan diet can get it to regress or at least not grow. But ulcerative colitis I had not seen—I guess because I’m a cardiologist I don’t always go into other literature. The study said there was a 100% remission rate in one year on a vegan diet, 90% at two year—with no drugs.
Q: It doesn’t seem like people get the message. Will they ever?
I kind of look at it as a jigsaw puzzle you’ve got a piece there and a piece there and slowly people are sort of putting it together.
Q: What have you done at ACC to advance the vegan diet?
One of our victories at ACC involved the federal USDA nutrition guidelines. They had misquoted our recommendations on cholesterol. We had said more research was needed but we never meant they should remove the recommended daily limit of 300 mg. So we gave them a massive amount of literature. We were saying “Oh please don’t remove that 300 mg limit—people are going to go hog wild," no pun intended.
(Williams in full ACC presidential garb photo at left)
Q: But there’s no cholesterol limit stated now in the guidelines, right?
They removed the 300 mg limit for the opposite reason. [Instead of setting a maximum ceiling for cholesterol consumption] They said one should eat as little cholesterol as possible, that the goal should be to eat zero cholesterol if you can. We are really happy with that, it’s better than what we were asking for.





