Article
We Don't Control the Numbers
While we are increasingly evaluated on numbers-A1c, blood pressure, LDL-these parameters are largely outside of our direct control. Mr M is a case in point.
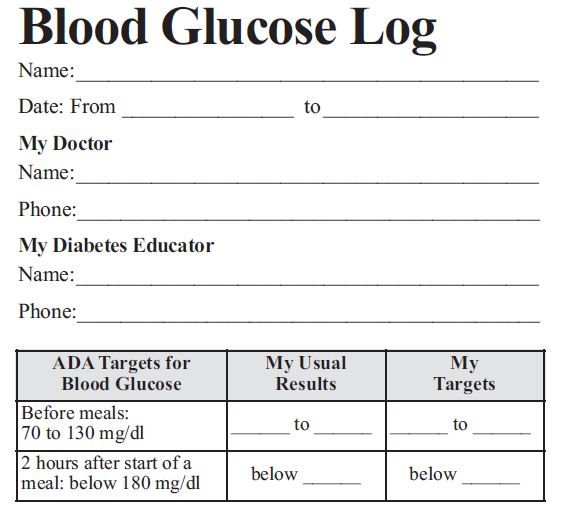
Glucose log, courtesy of American Diabetes Association.
How many of you can relate to this scenario?
I was about to see Mr M for a follow-up visit for his type 2 diabetes (T2DM). His A1c is not at goal, and he has been having challenges with self-management. I don’t think he’s ever brought in his SMBGs. After exchanging a couple of comments on hobbies, or other pleasantries, I always pose similar questions to all our patients with diabetes: “Have you been testing your blood sugars?” “Did you bring your log book today?” More often than not, I get a sheepish response. This patient, unfortunately, was no exception. “I’m sorry, Doc, I forgot.” I’ve also heard from others, “I lost my meter a long time ago.” “I just haven’t had time to test (or to record) my readings.” On further questioning, it turns out to have been 6 or more months since the patient lost a meter or it broke down irreversibly!
Or you see that the last time their metformin or Lantus was filled was 1 year ago. What is really happening here? Are these individuals simply what many would term “non-compliant”? Should we just quietly chart for the umpteenth time that the patient did not bring the glucometer, or the updated log book, and resign ourselves to the thought that the best we can hope for is not going over an A1c of 9%?
Before you throw your hands up, please consider this. Have you tried to meet your patients where they are? What fears, misconceptions, or gaps in knowledge do they have?
One tool that may help is “salient belief analysis.” You ask the patient, “Please tell me what comes to mind when you think of _____.” This blank could be filled in with "diabetes," "taking insulin," "testing your glucose," or "bringing your readings." Then simply listen with an open mind to what s/he says. The responses serve as a springboard for further discussion on ways to address the patient’s fears, barriers, and concerns.
I learned this tool earlier this month in a patient education class my colleagues and I were sent to, for improving our skills. The facilitator said, “I really encourage you all to give this one a try.” So I did, with Mr M. I was curious to hear how he would respond. Mr M simply replied, after a brief pause, “I think it’s just me being lazy.” I encouraged any other thoughts, but he didn’t have any other reasons. After asking him who or what may help offer a potential solution, he noted, “My wife!” He did seem more engaged during the rest of the visit, as he started thinking more in terms of solutions. I’m interested to see if he’ll enlist her assistance.
While we are increasingly being evaluated on numbers-A1c, blood pressure, LDL-these parameters are largely outside of our direct control. Sure, we can advise, encourage, or offer support, and we should. But we all know, ultimately, it’s up to the patient living with diabetes. Being willing to try approaches that draw out the patient can facilitate both a better clinic experience as well as improved clinical outcomes-for both patient and physician alike.




