Publication
Article
Family Practice Recertification
A Reassuring EKG... Not For Long
Author(s):
A 51 year-old man with a history of well-controlled hypertension presents to his primary physician's office for an acute care visit with chest discomfort that would come and go.
A 51 year-old man with a history of well-controlled hypertension presents to his primary physician’s office for an acute care visit with chest discomfort that would come and go. It began the previous day after dinner and he thought might have been caused by reflux. He never had reflux before and his wife was not satisfied with the self-diagnosis and therefore urged him to visit his doctor.
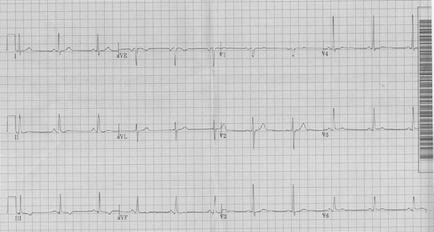
He did not appear in any distress. The pain had come and gone a couple times in the morning, lasting 5-10 minutes at a time, but he had no pain in the clinic. His heart rate was 70 beats per minute and his blood pressure was 138/84. His exam was normal and an EKG obtained in the office is shown below.
EKG1
He had no prior EKG for comparison. Despite the patient’s pain being gone, the physician recommended his patient get to the emergency department for further evaluation. The patient refused. So his physician drew a CBC, basic chemistry and troponin. The patient left.
Approximately 60 minutes later, after returning to work, the patient’s pain began to return and was unremitting. This coincided with the time the troponin value returned at 0.17 (nl<0.05). The patient was told to call 911.
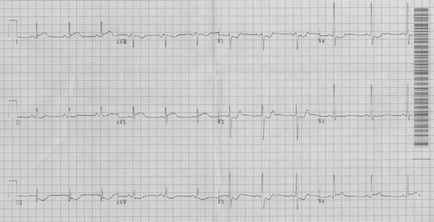
His arrival EKG is shown below.
EKG2
There is a stark difference between the first and second EKG. Regardless of how either EKG is read, we now have a man with coronary risk factors, chest pain and dynamic EKG changes with symptoms.
The eye-catching changes in EKG 2 are the ST depressions in the anterior (V3-V4) and septal (V1-V2) leads. He also has ST and T wave abnormalities in the inferior leads. But the changes that should lead you to immediately activate the cardiac catheterization lab, or consider thrombolytics if a cardiac catheterization lab is not available, is the ST elevation seen in the lateral leads (I, aVL and V6) consistent with acute myocardial infarction (MI).
Although the diagnosis of ST elevation MI (STEMI) was already made and the catheterization laboratory had been activated, a posterior EKG was performed and is shown below.
EKG 3
The leads for V5-V6 were removed and placed in the alternative positions required to obtain a posterior EKG. A posterior EKG is performed by extending the precordial leads beyond V6 to the back. V6 ends in the lateral axillary line. V7 (posterior axillary line) would continue posteriorly on the patient’s back as would V8 (midscapular) and V9 (paraspinal). The limb leads and V1-V3 are unchanged in a posterior EKG.
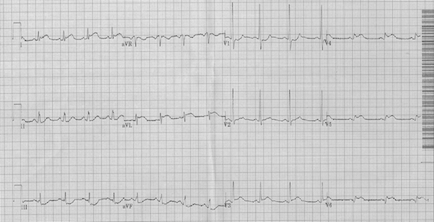
A posterior EKG is most helpful in diagnosing coronary obstruction resulting in myocardial infarction when the standard EKG does not diagnose STEMI but suspicion for a closed coronary artery is high. Supporting EKG features of an isolated posterior MI on a standard 12 lead are seen in the anteroseptal leads (V1-V3) including horizontal or down-sloping ST segment depressions, R waves greater than 0.04 seconds, R/S ratio > 1 and upright T waves. In the appropriate clinical scenario, this is highly suggestive of a posterior MI and posterior leads can clinch the diagnosis. However, a broad R wave or an R/S ratio > 1 in V1 can also be seen in some cases of right bundle branch block, Wolff-Parkinson-White syndrome, right ventricular hypertrophy and other conditions listed below.
Isolated posterior MI is uncommon (3-11%) of infarcts, but often accompanies an inferior MI or lateral MI. When posterior MI (lacking obvious ST segment elevation) is in isolation, it requires a high degree of suspicion to avoid missing the diagnosis so that emergent revascularization may be provided. Isolated posterior MI has been associated with door-to-activation times twice that of other STEMI and fewer patients obtaining coronary reperfusion within the recommended 90 minute time frame.
Because of the ST elevations in the lateral leads of our patient, posterolateral STEMI was easily diagnosed and the patient was taken emergently to the cardiac catheterization laboratory where a proximal left circumflex acute occlusion was identified. Percutaneous revascularization with a drug-eluting stent was performed and the patient was discharged without complication.
EKG findings in V1-V2 in isolated posterior myocardial infarction:
1. ST segment depressions with upright T waves
2. R wave duration > 0.04 seconds
3. R/S ratio > 1
Differential diagnosis of a R/S ratio > 1:
1. Right bundle branch block
2. Ventricular ectopy
3. Right ventricular hypertrophy
4. Acute right ventricular dilation (strain)
5. Posterior MI
6. Hypertrophic cardiomyopathy
7. Muscular dystrophy
8. Dextrocardia
9. Normal variant (<1% population)
10. Misplaced precordial leads
Triaging chest pain in clinic and deciding who needs to be urgently transferred to the emergency department can be challenging. EKGs are often obtained, but it should be recognized that they are snapshots in time and can evolve quickly. A normal, or near normal EKG with symptoms concerning for acute coronary syndrome should prompt referral to emergency department, or a call to 911. Biomarkers are helpful, but can take time to be resulted, increasing the time to appropriate therapy. Consider serial EKGs performed 15 minutes apart to evaluate concerning symptoms. And lastly, posterior ECGs can be helpful in finding otherwise electrically silent isolated posterior STEMI.
Mattu A, Brady WJ, Perron AD, Robinson DA. Prominent R wave in lead V1: electrocardiographic differential diagnosis. Am J Emerg Med. 2001 Oct;19(6):504-13
Perloff JK. The recognition of strictly posterior myocardial infarction by conventional scalar electrocardiography. Circulation. 1964 Nov: 706-719
Waldo Sw, Armstrong EJ, Kulkarni A, hoffmayer KS, Hsue P, Ganz P, MCabe JM. Clinical characteristics and reperfusion times among patients with an isolated posterior myocardial infarction. J Invasive Cardiology. 2013 Aug; 25(8):371-5






