Publication
Article
Family Practice Recertification
A Young Woman with Right Hip Pain
Author(s):
Since pain typically presents before bone lesions are displayed on radiographs, a true diagnosis may be overlooked and the early stages can be easily missed.
James D. Collins, MD
This 24-year-old woman presented with the complaint of right hip pain that she has had for 2 years. She described the pain as deep and persistent, radiating to her right buttocks and anterior thigh, and increasing in severity at night, though its distribution was nonsciatic. Although muscle rubs and heat did not relieve the pain, it resolved completely with aspirin administration.
The patient continually increased the dosage and at presentation, she was taking 600 mg of aspirin every 3-4 hours. Her physical examination findings were essentially negative, save for the aching and tender right hip.
Radiographic Findings
The woman’s anterior-posterior (AP) pelvis radiograph (Figure 1) displayed a small, round, radiolucent lesion marginated by an area of increased bone density in the cortical margin of the right femur adjacent to the lesser trochanter.

Figure 1
This AP radiograph displays the characteristic small, round, radiolucent lesion of osteoid osteoma (arrows) marginated by an area of increased bone density within the cortical margin of the femur. F=femur.
An AP radiograph of her right femur (Figure 2) displayed the same findings, while an enlarged AP view (Figure 3) provided greater detail of the central lucency and marginal sclerosis. A technetium-99m (Tc-99m) bone scan (not illustrated) was positive with intense scintigraphic activity in the central nidus and less intense activity in the area of peripheral sclerosis.

This AP view displays the right femur with the radiolucent nidus (bar arrow) surrounded by increased bone density within the cortical margin of the femur (arrows).
Figure 2
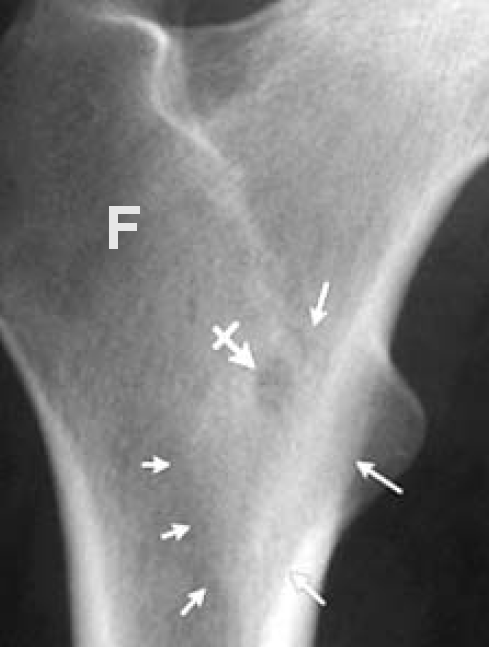
Figure 3 This enlarged AP view clearly defines the central lucency of the lesion (bar arrow) and marginal sclerosis (small arrows).
Diagnosis
Clinical considerations in the differential diagnosis included osteomyelitis, osteoblastoma, osteochondritis, stress fracture, and aseptic necrosis. A biopsy conducted 2 weeks after the radiographs were completed confirmed the diagnosis of osteoid osteoma.
Discussion
Osteoid osteoma is a benign osteoblastic lesion consisting of vascular osteoid tissue centrally and sclerotic bone peripherally. This type of osteoblastic lesion is commonly found in the diaphysis of long bones, such as the femur or tibia, although it can also occur more rarely in the bones of the hands, feet, and posterior spine. The lesion is usually round or ovoid and smaller than 1.5 cm in diameter, though its size can range from 0.5-2.0 cm. It occurs predominantly in children, adolescents, and young adults up to 25 years old and has a roughly 2:1 male-to-female ratio.
Localized, nocturnal pain is characteristic of osteoid osteoma, and patients may also experience vasomotor disturbances like flushing. In most cases, salicylates completely relieve symptoms.
Unlike osteoid osteoma, osteoblastoma is associated with variable pain and more often affects the axial skeleton, as approximately one-third of the benign bone lesions occur in the spine. Additionally, osteoblastomas are generally larger than osteoid osteoma and have a less well-defined sclerotic border.1 Osteomyelitis usually has a larger peripheral area of radiolucency due to increased edema and necrosis.2
Definitive treatment for osteoid osteoma requires surgical excision, percutaneous thermocoagulation, or radiofrequency ablation guided by either computed tomographic (CT) or magnetic resonance imaging (MRI). One advantage of MRI is that it displays fascial plane landmark anatomy beyond what CT can display. Percutaneous techniques are usually preferred over open surgical excision because they have fewer complications and shorter recovery time.
Take-home Message
Since pain typically presents before bone lesions are displayed on radiographs, a true diagnosis may be overlooked and the early stages can be easily missed. The key to the diagnosis of osteoid osteoma is tenderness over the site and complete pain relief following aspirin administration.3,4
References
1. Greenspan A. Benign bone-forming lesions: Osteoma, osteoid osteoma, and osteoblastoma. Clinical, imaging, pathologic, and differential considerations. Skeletal Radiol. 1993;22:485-500.
2. Miller SL, Hoffer FA. Malignant and benign bone tumors. Radiol Clin North Am. 2001 Jul;39(4):673-99.
3. Rosenthal DI, et al. Osteoid osteoma: Percutaneous treatment with radiofrequency energy. Radiology. 1993 Oct;229:171-175.
4. Cantwell CP, et al. Current trends in treatment of osteoid osteoma with an emphasis on readiofrequency ablation. Eur Radiology. 2004 Apr; 14:607-617.
About the Author
James D. Collins, MD, is Professor and General Radiologist in the Department of Radiology at the UCLA David Geffen School Medicine. He formerly served as Director of the required medical student training for the department and President of the James T. Case Radiologic Foundation. Collins has an extensive background of publications, consultations, and editorial positions, including his current post as the Radiology Editor for the Journal of the National Medical Association. He specializes in bilateral 3-dimensional MRI and MRA imaging of the brachial plexus and has been performing those studies since 1985.