Publication
Article
Family Practice Recertification
Upper Chest Wall Lesion in a Middle-aged Woman
Author(s):
A 58-year-old woman presented to clinic with concerns about this skin lesion on her upper chest. She reports it has been present for 1 year and is slowly enlarging. The lesion is otherwise asymptomatic and her past history is only significant for rheumatoid arthritis (RA), for which she takes methotrexate and etanercept.
a) Seborrheic keratosis
b) Basal cell carcinoma
c) Benign nevus
d) Melanoma
e) Squamous cell carcinoma
Diagnosis
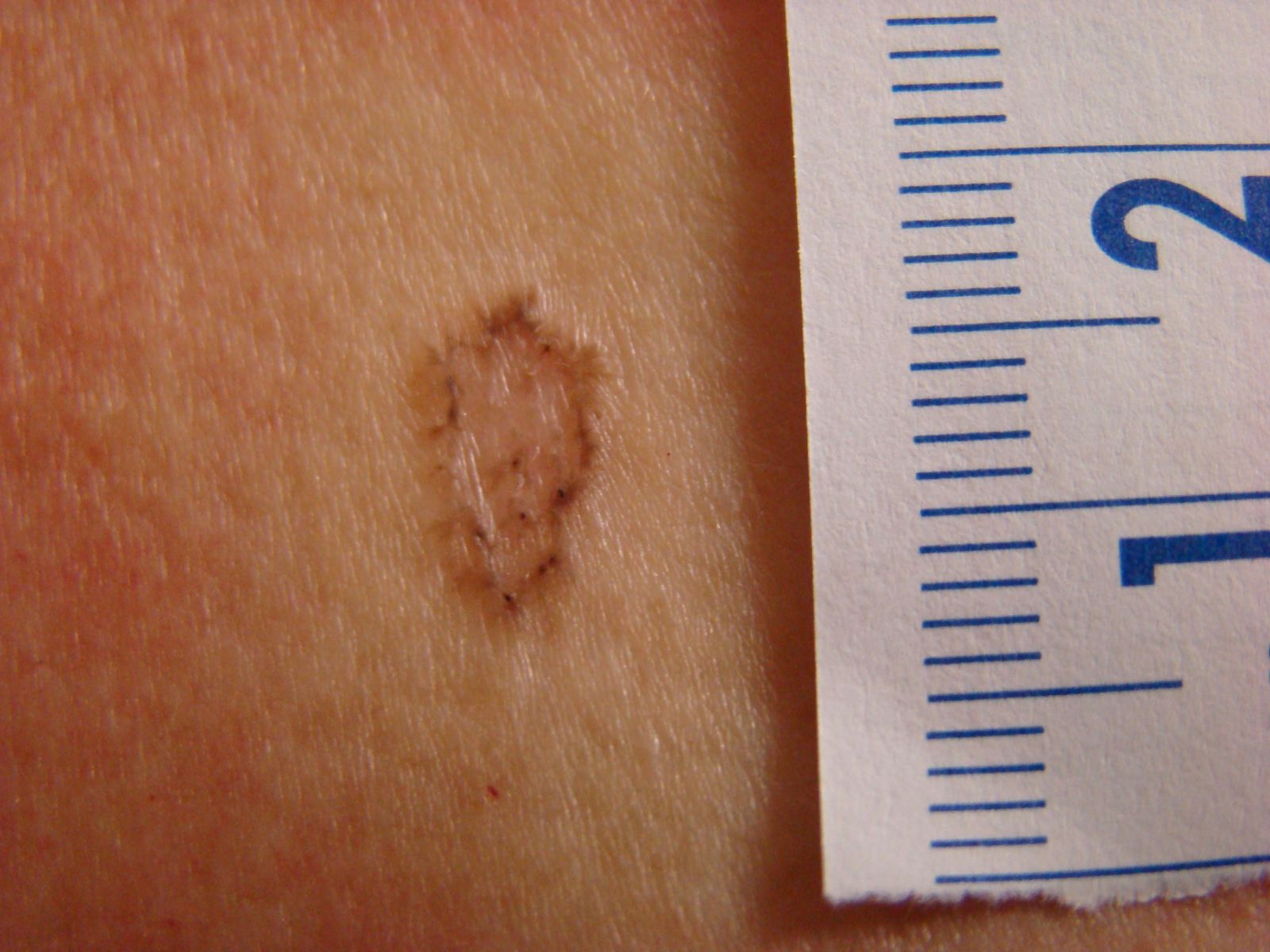
A deep shave biopsy confirmed this woman has pigmented basal cell carcinoma (BCC), the most common form of skin cancer. BCCs are characterized by raised or rolled borders — which can be seen on this lesion closest to the ruler — a waxy appearance, telangiectasias, and often erosion with poor healing. Although they are usually flesh colored, one single-center study found 7% of them were pigmented.1 When pigmented, BCCs are very difficult to clinically distinguish from melanoma. However, dermoscopy may be useful2 and biopsy is indicated for confirmation in either BCC or suspected melanoma.
Seborrheic keratoses typically develop after the third decade of life and are frequently seen on the trunk and face. They usually have a brown, hyperpigmented, and rough surface. As they often itch, the upper portion is commonly scratched off by the patient. This can leave a surrounding margin of hyperpigmentation with raised features akin to this lesion, though the patient’s history did not support it.
Benign nevi are extremely common, but they usually have a relatively uniform pigmentation with sharply demarcated borders. If the margins are raised, they tend to be higher in the middle, contrary to the raised borders of this lesion.
Melanoma must be included in the differential diagnosis of any pigmented lesion, especially if it is new and enlarging. Melanomas often have irregular borders, sometimes bleed or itch, and usually involve pigmentation that is dark or comprises more than one color in the same lesion. In diagnosing a melanoma, a deep shave biopsy is easier and quicker than a full thickness excision. Due to the danger of metastasis, it is very appropriate to perform a biopsy on this type of lesion at presentation, in order to avoid possibly losing a patient with melanoma to follow-up.
Squamous cell carcinoma has lesion presentations that range from scaly with underlying erythema, to raised and ulcerating. Bowen’s disease, or squamous cell carcinoma in situ, can appear as a more subtle, rough, or scaly lesion usually on sun-exposed areas, such as this woman’s upper chest.
References
1. Abbas OL, Borman H. Basal cell carcinoma: a single-center experience. ISRN Dermatol. 2012;2012:246542. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3539390/.
2. Menzies SW, Westerhoff K, Rabinovitz H, Kopf AW, McCarthy WH, Katz B. Surface microscopy of pigmented basal cell carcinoma. Arch Dermatol. 2000
Aug;136(8):1012-6. http://archderm.jamanetwork.com/article.aspx?articleid=190512.
About the Authors

Daniel Stulberg, MD, is a Professor of Family and Community Medicine at the University of New Mexico. After completing his training at the University of Michigan, he worked in private practice in rural Arizona before moving into full-time teaching. Stulberg has published multiple articles and presented at many national conferences regarding skin care and treatment. He continues to practice the full spectrum of family medicine with an emphasis on dermatology and procedures.
Andrew Larson, MD, is a graduate of the University of Arizona School of Medicine and currently a Family Medicine Resident at the University of New Mexico.