Publication
Article
Cardiology Review® Online
Association of HDL Cholesterol With Incident Cardiovascular Events in Women, by LDL Cholesterol and Apo B100 Levels

Sucheta Gosavi, MD
Review
Mora S, Buring J, Ridker PM, Cui Y. Association of high-density lipoprotein cholesterol with incident cardiovascular events in women, by low-density lipoprotein cholesterol and apolipoprotein B100 levels: a cohort study. Ann Intern Med. 2011;55:742-750.
D
isturbances in lipid profile have been one of the major contributors to cardiovascular disease (CVD). Age, obesity, diabetes mellitus (DM), hypertension (HTN), smoking, and gender play a very important role in the development of lipid disorders. There are numerous published studies that have measured different types of cholesterol, triglycerides, apolipoprotein A-1 (apo A-1), and apolipoprotein B100 (apo B100), and have defined their relationship with CVD for both coronary artery disease (CAD) and stroke. CAD remains the major cause of death among American women, although it occurs later in life among women than among men. In men, it has been shown that the inverse relation of high-density lipoprotein cholesterol (HDL-C) with CVD persists irrespective of the level of low-density lipoprotein cholesterol (LDL-C). Whether or not this is true for women has not been well studied. The aim of this study was to establish an association of HDL-C, apo A-1, and CVD with all ranges of LDL-C and apo B100. Apo B100 includes all atherogenic particles: intermediate density lipoprotein (IDL), very low-density lipoprotein (VLDL), large LDL-C, and small dense LDL-C (sd LDL-C). The secondary aim of this study was to observe if very high HDL-C noted in some of the women confers any added CVD protection.
Study Details
The participants of this study were apparently healthy, white health care professional women, 45 years or older, who were randomized to either low-dose aspirin and vitamin E or to placebo for primary prevention of CVD and cancer (Women’s Health Study cohort). Basic demographics, anthropometric measurements, smoking, use of hormones, medical history, and lifestyle factors were documented and baseline lipid samples were collected at enrollment in the study. Direct measurements of HDLC
and LDL-C were performed and apo A-1 and apo B100 were measured by immunoassay. A total of 26,861 women met the study inclusion criteria.
The outcomes reported for CVD were nonfatal myocardial infarction, percutaneous intervention, coronary artery bypass graft, cardiovascular deaths, and stroke. These end points were determined by self-reporting in the followup questionnaire every 6 months for the first year, and then yearly for a mean of 11.1 years. These events were then corroborated by accessing medical records with permission, and only the confirmed events were included in the analysis.
For the analysis, HDL-C and apo A-1 levels were divided into quintiles ranging from <39.5 mg/dL to >61.6 mg/ dL for HDL-C and <1.24 g/L to >1.6 g/L for apo A-1. LDL-C and apo B100 were divided into tertiles ranging from <108 mg/dL to >135 mg/dL for LDLC and <0.90 g/L to >1.13 g/L for apo B100. All results were adjusted for age, race, randomized treatment assignment, smoking status, systolic blood pressure, antihypertensive medications, fasting status, alcohol use, family history of premature CAD, postmenopausal status, hormone replacement therapy, body mass index (BMI), exercise, DM,
and C-reactive protein and triglyceride (TG) levels.
At baseline, the mean HDL-C concentration was 54 mg/dL (SD, 15) and apo A-1 was 1.51 g/L (SD, 26). HDL-C and apo A-1 values were inversely related to the events of CVD and coronary events when stratified by age, race, HTN, smoking, DM, hormone use, and BMI.
The total number of CVD events was 929, of which 602 were coronary and
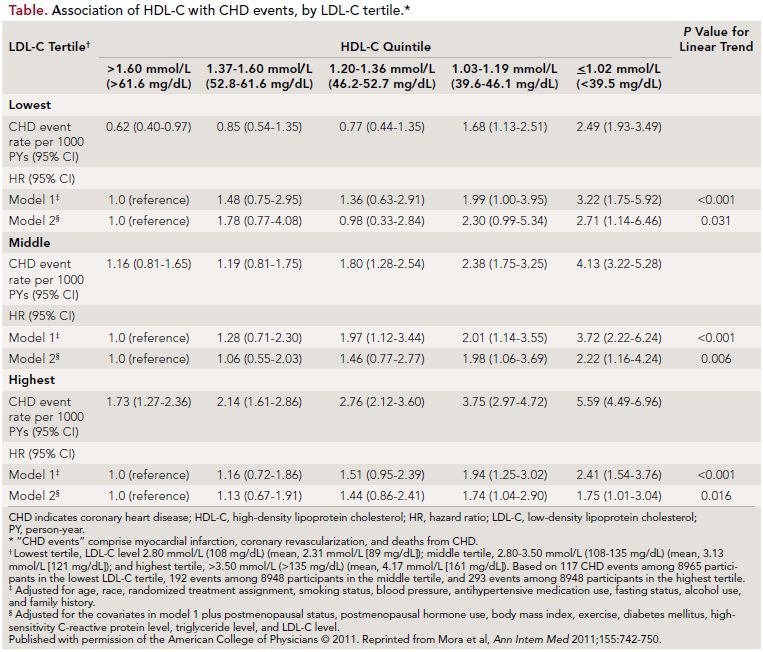
319 were strokes. There was a direct linear association between decreased HDL-C and increased CVD events (P <0.001); however, this association was found to be weaker for apo A-1. The association of HDL-C with CVD events remained statistically significant for a range of LDL-C, the lowest being <108 mg/dL and the highest being >135 mg/ dL, thus making HDL-C levels one of the important predictors for risk of cardiovascular events. In the lower HDL-C group, some of the well-known risk factors—
including HTN, DM, increased BMI, high LDL-C, high C-reactive protein, and smoking—were noted at a higher percentage (Table). The study also evaluated data for an
association between HDL-C and apo A-1 values across a range of apo B100 levels, and found a significant inverse association for coronary events but not
for stroke. This association for coronary events was found to be significant when the apo B100 levels were >0.9 g/L
(P <0.001).
Although no significant association was found between HDL-C or apo A-1 and stroke, the overall stroke risk was higher in the participants with the lowest
HDL-C level. It was noted that some of the women who developed CVD despite high HDL-C levels were older or had risk factors like HTN, DM, or increased LDL-C and TG levels. It was thus inferred that, above a certain level of HDL-C concentration (~57 mg/dL), the risk of CVD did not diminish further.
References
1. Walldius G, Junger I. The apo B/apo A-1 ratio: strong, new risk factor for cardiovascular disease and a target for lipid lowering therapy: a review of the evidence. J Intern
Med. 2006;259:493-519.
2. Barter P, Gotto AM, LaRosa JC, et al. HDL cholesterol, very low levels of LDL cholesterol and cardiovascular events. N Engl J Med. 2007;357:1301-1310.
3. deGoma EM, Leeper NJ, Heidenreich PA. Clinical significance of high-density lipoprotein cholesterol in patients with low lowdensity lipoprotein cholesterol. J Am Coll
Cardiol. 2008;51:49-55.
4. van der Steeg WA, Holme I, Boekholdt SM, et al. High-density lipoprotein cholesterol, high-density lipoprotein size, and apolipoprotein A1: significance for cardiovascular risk: the IDEAL and EPIC Norfolk studies. J Am Coll Cardiol. 2008;51:634-642.
COMMENTARY
Association of HDL With CardiovascularEvents in Women
This study has reinforced the known inverse association of HDL-C with CVD in a wide range of LDL-C levels in women. The authors have also included the relation of apo B100 (the atherogenic lipoprotein) and apo A-1 (athero-protective lipoprotein) with CVD, including stroke. Decreased total apo B100 has resulted in fewer cardiovascular events. However, apo A-1 had a weaker association with CAD and virtually no association with stroke.
A review of the literature shows that in the AMORIS and INTERHEART studies, high apo B100 and low apo A-1 were significantly associated with increased risk of CAD and stroke in both men and women.1 Analysis of the Treating to New Targets (TNT) study has found an inverse relationship between HDL-C and cardiovascular events with low LDL-C (<80 mg/dL) in both genders.2 The fact that low HDL-C carries an increased risk of CVD irrespective of the LDL-C levels has been previously noted in men.3
The EPIC NORFOLK study compared the ratio of LDL-C to HDL-C and apo B100 to apo A-1 and concluded that the apo B100 to apo A-1 ratio is a stronger predictor of the risk of future CAD.1 One of the reasons the apo B100 to apo A-1 ratio is a better indicator to risk-stratify CVD is that very high HDL-C levels and very large HDL-C particles have been shown to be atherogenic rather than atheroprotective.4
Although the study by Mora et al found a significant association of high HDL-C with a decreased risk of CAD and a weaker association of apo A-1 with CAD,
it did not find any significant association between HDL-C or apo A-1 with stroke. There have been several reports in the literature in which decreased HDLC values were associated with stroke. 1 It is possible that the risk of stroke is due not only to high LDL-C or low total HDL-C, but to increased very large HDLC- alpha3 particles, which have been shown to be atherogenic by the EPIC NORFOLK study.4 Thus, the HDL-C values may not reflect the true atheroprotective potential, making the apo B100 to apo A-1 ratio a better indicator of the risk for CAD and stroke.
Some of the major advantages of the Mora et al study were that it was done in a large population of exclusively women, who were followed for a long period of time with accurate measurements in a standardized laboratory. But since it was in a selected group of healthy white women who probably had a better-than-average lifestyle, the results may not be accurately extrapolated to the general population. Only 1 baseline lipid sample was taken, hence the change in HDL-C or LDL-C levels over a period of
many years—which would impact the outcome—was not reported.
In conclusion, therapy should not be targeted only for increasing HDL-C or decreasing LDL-C, but also decreasing apo B100 and increasing apo A-1. Lowering the total atherogenic burden, which is reflected by apo B100, should be an important target for therapy.
About the Author
Sucheta Gosavi, MD, practices medicine at Kaiser Permanente Medical Center in Walnut Creek, CA. She is board certified in internal medicine and echocardiography.
Dr Gosavi received her medical degree at R.G. Kar Medical College in Kolkata, India. She completed her postgraduate studies in internal medicine in India and at the University of Missouri Columbia. Dr Gosavi was a research fellow at Massachusetts General Hospital in the cardiac ultrasound laboratory. She also has a master’s degree in tropical medicine and public health.
