Article
Hypertensive Retinopathy Positively Correlated with Albuminuria in Analysis
Author(s):
An analysis of the China Stroke Primary Prevention Trial revealed the correlation was more notable when stratified by triglycerides levels and smoking status.
A recent cross-sectional analysis of hypertensive adults in the China Stroke Primary Prevention Trial indicated a positive correlation between albuminuria and hypertensive retinopathy.1
The prevalence of albuminuria among the indicated population with hypertension was slightly higher (11.1%) than the general population in China (9.4%), with investigators noting the correlation was greater when stratified by smoking status and triglyceride levels.
“Such a high proportion makes chronic kidney disease (CKD) a serious public health problem in China, and early detection is becoming particularly important” investigators wrote.1
An early biomarker of kidney injury, albuminuria is a risk factor for end-stage renal disease and progressive CKD, as well as an independent predictive factor for cardiovascular and all-cause mortality.
For this analysis, the investigators from the Department of Ophthalmology, Peking University First Hospital, assessed albuminuria and hypertensive retinopathy in adults in rural China. Data used in the analysis were from the multicenter, double-blind, and randomized China Stroke Primary Prevention Trial. Investigators conducted cross-sectional analyses of data obtained from the last follow-up in 2013.
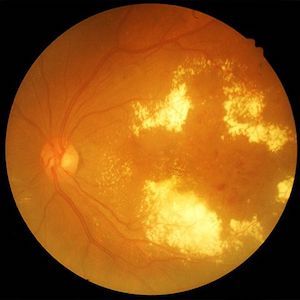
Among 3,860 adults with primary hypertension between 45 and 75 years of age with laboratory tests for albuminuria included in the study, 3,121 underwent fundus photography. In the testing, a urinary albumin to creatinine ratio (UACR) equal to or greater than 30 mg/g was identified as albuminuria. The study enrolled 2,964 subjects and used Keith-Wagener-Barker stages to assess the effect of hypertension on retina vessels.
Upon analysis, data show hypertensive retinopathy in 76.6% (n = 2,271) of participants, and albuminuria in 11.1% (n = 330). After adjusting for relevant factors, UACR levels were significantly higher in subjects with hypertensive retinopathy than those without (grade 1, β = 1.42, 95% confidence intervals [CI]: -0.12 – 2.95; P = .070; grade 2, β = 2.62, 95% CI: 0.56 – 4.67; P = .013; grade 3, β = 5.17, 95% CI: 1.13 - 9.20; P = .012).
Moreover, there were significant interactions when data were stratified by triglycerides (P for interaction = .023) and smoking status (P for interaction = .014). The study reported stronger correlations between UACR and hypertensive retinopathy in participants with higher triglyceride levels (≥1.7 mmol/L). For grade 3 hypertensive retinopathy, a strong correlation between UACR and hypertensive retinopathy was found in subjects with lower triglyceride levels (<1.7 mmol/L; P for interaction = .023).
Results indicated a significant interaction when data were stratified by triglyceride level (P for interaction = .014). There was a strong correlation between albuminuria and hypertensive retinopathy grades 1 and 2 in subjects with higher triglyceride levels (grade 1, odds ratio [OR] = 1.57; 95% CI, 1.08 - 2.29; P = .019; grade 2, OR = 2.02; 95% CI, 1.28 - 3.18; P = .002. For grade 3, a strong correlation between albuminuria and hypertensive retinopathy was observed in subjects with lower triglyceride levels (OR = 2.7; 95% CI, 1.09 - 6.73).
Investigators reiterated the need for improved screening to better detect CKD in the population and plan to continue to follow the study cohort to collect more endpoint data for analysis.
“These results highlight the need for albuminuria screening in hypertensive patients complicated with hypertensive retinopathy to ensure early detection of CKD,” they wrote.1
References
- Li, J., Zhang, W., Zhao, L. et al. Positive correlation between hypertensive retinopathy and albuminuria in hypertensive adults. BMC Ophthalmol 23, 66 (2023). https://doi.org/10.1186/s12886-023-02807-6
2 Commerce Drive
Cranbury, NJ 08512
All rights reserved.




