Publication
Article
Cardiology Review® Online
Lowering LDL Cholesterol With Statin Therapy in Low-Risk Populations

Chrisandra Shufelt, MD, MS, NCMP
Review
CTT Collaborators. The effects of lowering LDL cholesterol with statin therapy in people
at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials.
Lancet. 2012;doi.10.1016/SO140-6736(12)60367-5.
Intensive lowering of LDL cholesterol has previously been found to reduce major vascular events by 20%.1 However, questions still remain about the use of statins for primary prevention and in low-risk individuals. This recent meta-analysis by the Cholesterol Treatment Trialists’ (CTT) Collaborators sought to answer these questions by comparing 134,537 patients (median follow-up of 4.8 years) in trials of statins versus controls, and 39,612 patients (median follow-up of 5.1 years) in trials of low-dose versus high-dose statin therapy.2 The baseline 5-year risk of a major vascular event (MVE) was determined for each participant and stratified into categories (<5%, ≥5% to <10%, ≥10% to <20%, ≥20% to <30%, >30%), with MVE, defined as nonfatal myocardial infarction, coronary death, coronary revascularization, or stroke. The analysis calculated the rate ratio (RR) per 1 mmol/L of low-density lipoprotein (LDL) cholesterol lowering.
Overall, the investigators found that lowering LDL cholesterol by 1 mmol/L (39 mg/dL) decreased the risk of MVE by 21%, irrespective of age, sex, baseline LDL cholesterol values, or previous vascular disease. All risk groups benefited from statin therapy (Table). Remarkably, the risk reduction was lowest in the lowest-risk categories, with a 38% reduction of MVE in the <5% group. This reduction corresponds to an absolute risk reduction of MVE of 11 events per 1000 patients for every 1 mmol/L (39 mg/dL) LDL reduction for individuals with a baseline risk of <10%. The study also stratified the analysis by individuals with or without a history of cardiovascular disease, and found that statins had comparable results in the 2 groups, reducing MVE (RR 0.75; 95% CI, 0.70-0.80), vascular mortality (RR 0.85; 95% CI, 0.77-0.95), and all-cause mortality (RR 0.91; 95% CI, 0.85-0.97) in individuals without a history of cardiovascular disease. Overall, a reduction in stroke risk was seen (RR 0.85; 95% CI, 0.80-0.89) and the reduction in risk among subjects with <10% baseline risk was similar to that in higher-risk categories (P for trend = 0.3). Finally, the study also evaluated cancer incidence and cancer deaths with statin use and found no increased risk.
References
1. Cholesterol Treatment Trialists’ Collaboration. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trails. Lancet. 2010;376:1670-1681.
2. Cholesterol Treatment Trialists’ Collaborators. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomized trials. Lancet. 2012;doi.10.1016/SO140-6736(12)60367-5.
3. Gutierrez J, Ramirez G, Rundek T, Sacco RL. Statin therapy in the prevention of recurrent cardiovascular events. Arch Intern Med. 2012;172:909-919.
4. Sattar N, Preiss D, et al. (2010). Statins and risk of incident diabetes: a collaborative meta-analysis of randomised statin trials. Lancet. 375:735-742.
5. Kerr AJ, Broad J, Wells S, Riddell T, Jackson R. Should the first priority in cardiovascular risk management be those with prior cardiovascular disease? Heart. 2009;95:125-129.
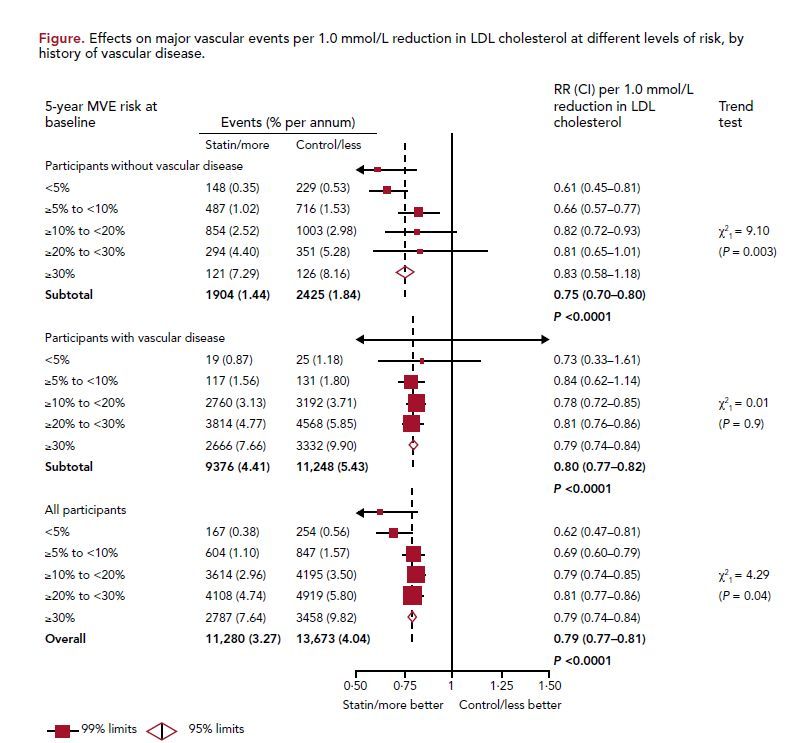
Heterogeneity between participants without and with vascular disease: χ2
1 = 2.74 (P = 0.10)
MVE, major vascular event; RR, rate ratio; CI, confidence interval.
Reprinted from The Lancet, doi:10.1016/S0140-6736(12)60367-5, Cholesterol Treatment Trialists’ (CTT) Collaborators, “The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials.” Published online May 17, 2012. Copyright 2012, with permission from Elsevier.
COMMENTARY
Impact of Statins on Reduction of Vascular Events
This study adds to the growing body of evidence that statin therapy has a significant impact on the reduction of vascular events that is attributable to LDL lowering. The authors suggest that given this substantial risk reduction in low-risk individuals, LDLlowering guidelines in this population may need to be reconsidered. The cornerstone of primary prevention is to first recommend lipid lowering for the at-risk population through lifestyle changes such as diet, weight loss, and exercise. Medication guidelines are considered when such changes are not adequately effective and include statin therapy, with additional pharmacotherapy as needed. Current guidelines
are based on the goal of reducing LDL levels, no matter what the means.
It was disappointing that the authors did not present an analysis stratified by sex to address whether results were comparable in men and women. A recent meta- analysis by Gutierrez and colleagues3 in the Archives of Internal Medicine provided a sex-based analysis of secondary prevention trials, concluding that the reduced risk of CVD with statins was comparable in women (RR = 0.81; 95% CI, 0.74-0.89) and men (RR = 0.82; 95% CI, 0.78-0.85). Whether these results also apply to the primary prevention setting and low-risk populations remains uncertain. Moreover, Gutierrez et al found that statins significantly reduced stroke and all-cause mortality in men but not in women.3 In the low-risk populations in the present meta-analysis, it would have been helpful to have had a comparison arm with LDL lowering through lifestyle modifications without statin therapy. This would have further differentiated whether statin therapy has benefits beyond LDL lowering. One may hypothesize that the reduction in MVE and all-cause mortality seen in the low-risk population may not be wholly attributable to LDL reduction, but also may be due to the decrease in inflammation related to statins. It is well-known that statin therapy lowers inflammatory markers, and inflammation is implicated in both cardiovascular and nonvascular disease processes.
In order to achieve a reduction in MVE as shown in this meta-analysis, individuals have to lower LDL by 1 mmol/L (39 mg/dL). Although most statins achieve significant LDL lowering, statin therapy is not a one-sizefits- all medication, and individual responses to statins vary. Lack of response may be due to differences in metabolism, polypharmacy, or medication noncompliance. Statin therapy also has known side effects such as myalgias and liver enzyme abnormalities. More recently, in another meta-study published in The Lancet, a slight increase in type 2 diabetes was found with statin use.4 The authors noted the incidence of diabetes in primary prevention trials was 5% per 5-years, or about 0.1% per 1000, much lower than the cardiovascular benefit seen from statins. Certainly there are risks and benefits involved with taking any medication.
Today, over half of cardiovascular events occur in lowrisk individuals with no previous history of vascular disease. 5 It is difficult to argue with the dramatic reduction in vascular events with statin therapy in both primary and secondary prevention populations and the relatively small numbers needed to treat. With anticipated updates in the National Cholesterol Education Program Adult Treatment Panel IV guidelines due to be released later this year, the prediction is that the LDL goal may in fact be lowered
for primary prevention. While this current meta-analysis supports the need to reassess lipid-lowering guidelines, future studies should focus on (1) whether MVE lowering in a low-risk population applies to all LDL-lowering methods or is reserved for statin therapy; (2) whether results apply equally to men and women; and (3) whether allcause mortality is also reduced.
About the Authors
Chrisandra Shufelt, MD, MS, NCMP, is the Associate Director of the Women’s Heart Center and Preventive and Rehabilitative Cardiac Center at the Heart Institute at Cedars-Sinai Medical Center, Los Angeles, CA, and Assistant Professor, Cedars-Sinai Medical Center. She was assisted in the writing of this article by JoAnn E. Manson, MD, DrPH, NCMP, FAHA , Chief of the Division of Preventive Medicine at Brigham and Women’s Hospital and Professor of Medicine and the Michael and Lee Bell Professor of Women’s Health at Harvard Medical School, Boston MA. Dr Manson has been Principal Investigator (PI) of the Boston center for the Women’s Health Initiative (WHI) since study inception in 1993, PI of the CVD component of the Harvard Nurses’ Health Study for 12 years, and PI of the recently launched VITamin D and OmegA-3 TriaL (VITAL).






