Publication
Article
Cardiology Review® Online
Sleep Apnea and Hypertension: The Impact of CPAP Treatment

Ragavendra Baliga, MD, MBA, FACP, FRCP (Edin), FACC
Review
Marin JM, Agusti A, Villar I, et al. Association between treated and untreated obstructive sleep apnea and risk of hypertension. JAMA. 2012;307:2197-2198.
Barbé F, Durán-Cantolla J, Sánchez-de-la-Torre, et al; for the Spanish Sleep and Breathing Network. Effect of continuous positive airway pressure on the incidence of hypertension and cardiovascular events in nonsleepy patients with obstructive sleep apnea: a randomized controlled trial. JAMA. 2012;307:2161-2168.

In the same issue of the Journal of the American Medical Association, 2 Spanish studies investigated obstructive sleep apnea (OSA) and the effect of treatment with continuous positive airway pressure (CPAP). The potential role of CPAP in preventing new-onset hypertension and cardiovascular events was also explored.
The first study by Marin et al1 was a prospective, observational study of 1889 individuals without elevated blood pressure, referred for nocturnal polysomnography between January 1, 1994, and December 31, 2000. Among these individuals, 1579 subjects were diagnosed with OSA. In this cohort, 824 were eligible for and adhered to CPAP treatment, whereas the remaining 755 were either ineligible for CPAP treatment according to national treatment guidelines, or were eligible but declined CPAP therapy, or were eligible and started CPAP but were nonadherent.
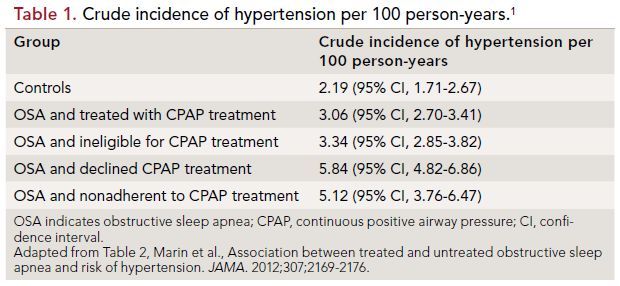
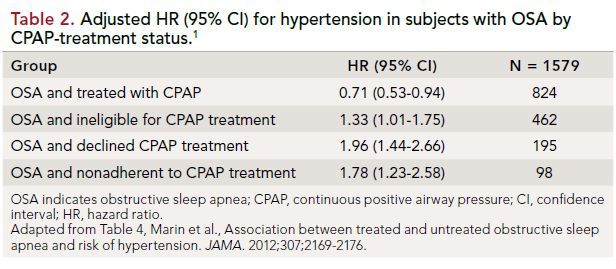
The investigators found that in the median follow-up period of 12.2 years, 37.3% (n = 705) developed hypertension. The study found that when compared with individuals without OSA, treatment with CPAP was associated with a lower risk of new-onset hypertension, whereas untreated OSA was associated with an increased risk of new-onset hypertension (Tables 1 and 2). This study suggests that OSA may be a modifiable risk factor for hypertension.
The study by Barbé et al2 evaluated the impact of CPAP treatment on the incidence of hypertension or cardiovascular events in 725 individuals with OSA (as evidenced by an apnea-hypopnea index of >20 per hour) who lacked symptoms of daytime somnolence (as evidenced by an Epworth Sleepiness Scale score of 10 or less).
The main outcomes were incidence of either systemic hypertension (BP>140/90 mmHg or taking antihypertensive drug therapy) or cardiovascular event (nonfatal myocardial infarction, nonfatal stroke, transient ischemic attack, hospitalization for unstable angina or arrhythmia, heart failure, or cardiovascular death).
In this randomized, controlled multicenter trial, there were 357 adults in the CPAP treatment group and 366 in the control group (usual care); the median follow-up duration was 4 years. During this period there were 68 cases of new hypertension and 28 cardiovascular events in the CPAP group, compared with 79 cases of new hypertension and 31 cardiovascular events in the control group. The incidence of new hypertension or cardiovascular events per 100 person-years in the CPAP group was
9.20 (95% CI, 7.36-11.04), whereas in the control group the incidence of new hypertension or cardiovascular events per 100 person-years was 11.02 (95% CI, 8.96-13.08) (incidence density ratio 0.83; 95% CI, 0.63-1.1; P = 0.20).
Therefore, in the CPAP group there was, at best, a trend toward a reduction in the incidence of hypertension and cardiovascular events that did not reach statistical significance. A post hoc analysis suggested that CPAP therapy may reduce the incidence of hypertension or cardiovascular events in individuals with CPAP adherence of 4 hours or longer every night.
References
1. Marin JM, Agusti A, Villar I, et al. Association between treated and untreated obstructive sleep apnea and risk of hypertension. JAMA. 2012;307:2169-2176.
2. Barbé F, Durán-Cantolla J, Sánchez-dela- Torre, et al; for the Spanish Sleep and Breathing Network. Effect of continuous positive airway pressure on the incidence of hypertension and cardiovascular events in nonsleepy patients with obstructive sleep apnea: a randomized controlled trial. JAMA. 2012;307:2161-2168.
3. Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560-2572.
COMMENTARY
The Impact of CPAP Obstructive Sleep Apnea
Both studies are important in that they better define the impact of CPAP in individuals with OSA. The study by Marin et al1 clearly suggests there is a causal role between OSA and hypertension and, more importantly, suggests that modifying OSA with CPAP therapy not only reduces blood pressure but favorably reduces the risk of developing hypertension. The study by Barbé et al2 is an important hypothesis-generating study because it suggests that treating OSA with CPAP therapy in patients without excessive daytime somnolence may reduce the risk of hypertension. The post-hoc analysis also suggested that CPAP therapy >4 hours duration every night was associated with a 3-mm reduction in systolic blood pressure. This is a significant change because a 3-mmHg reduction in systolic blood pressure is associated with an 8% reduction in stroke-related annual mortality, a 5% reduction in coronary heart disease- related annual mortality, and a 4% reduction in total annual mortality (Table 3).3
However, there are several issues that remain to be addressed: (1) predicting which patients with OSA are at risk of developing hypertension, secondary pulmonary hypertension, heart failure, and atrial fibrillation; (2) predicting which patients with OSA will favorably respond to CPAP (the responders); (3) finding the optimal duration of CPAP to have a significant therapeutic effect; (4) defining the risks and benefits of CPAP therapy in those without daytime sleepiness; and (5) discovering the mechanism
of blood pressure reduction with CPAP. To address these questions, a large multicenter, randomized, controlled trial will be required, with particular attention not only to the quality of life but also to morbidity (including hypertension, pulmonary hypertension, atrial fibrillation, and heart failure) and mortality in this cohort.
About the Author
Ragavendra Baliga, MD, MBA, FACP, FRCP (Edin), FACC, is Chief Mentor Officer for Clinical Faculty and Vice- Chief/Assistant Division Director, Division of Cardiovascular Medicine, Wexner Medical Center, and Professor of Internal Medicine at The Ohio State University in Columbus. He received his MD from St John’s Medical College in Bangalore, India, and completed his Internal Medicine residency at Victoria Hospital in Bangalore. He completed his Cardiology fellowship from Hammersmith Hospital, London, UK, and advanced fellowships from Brigham & Women’s Hospital/Harvard Medical School, Boston University Medical Center, and UT Southwestern Medical Center, Dallas, TX. He is board-certified in internal medicine and cardiovascular diseases. He was a faculty cardiologist at the University of Michigan and received an MBA from the Stephen Ross School of Business. Dr Baliga joined The Ohio State University in 2005.
