Sharing Decisions in Gout: Better Communication for Better Outcomes
More effective communication can improve both adherence to and outcomes of gout treatment regimens.
ABSTRACT: More effective communication can improve both adherence to and outcomes of gout treatment regimens. All patients should share with their physician a commitment to maintaining a serum urate concentration lower than 6 mg/dL. More important than limitation of exogenous, dietary purines is restriction of constituents that accelerate endogenous purine synthesis. An arthrocentesis often is useful in therapy and always is desirable for diagnosis. Improved understanding may help clinicians and patients overcome reluctance about aspiration. Patients must recognize that flares become more likely as hyperuricemia comes under control and that prophylactic anti-inflammatory therapy may be needed throughout this period of increased risk. Patients often remain uncertain about how or why they should take each medication for their gout. (J Musculoskel Med. 2008;25:116-123).

Gout stands virtually alone among the chronic rheumatologic diseases in that it has a pathognomonic diagnostic test, a reasonably well-understood pathogenesis,and an array of effective therapeutic interventions.1,2 In spite of these positive aspects, gout frequently is undertreated and mistreated.
Many failures in gout management may be attributed to miscommunication between harried physicians and their busy, seemingly recovering male patients. Both parties to physician-patient interactions need to recognize gout as a progressive condition, one that almost always can be controlled readily at its outset but without such control too often becomes more and more refractory and disabling as the years of neglect go by.
Once established, gout will remain a constant companion for the remainder of the patient’s life. Whether that presence is the pale shadow of well-controlled hyperuricemia or the vicious demon of chronic, tophaceous disease often is determined by the patient’s degree of adherence to a well- designed program. In this article, I address key issues in gout management and discuss how more effective patient-physician communication can improve adherence and medical outcomes.
MAINTAINING THE SERUM URATE LEVEL
The simple principle of crystal precipitating from supersaturated body fluids underlies the understanding of gout and much of its management. Every patient should know this principle well and should share with his or her physician a commitment to attaining and maintaining a serum urate concentration lower than 6 mg/dL (Figure).
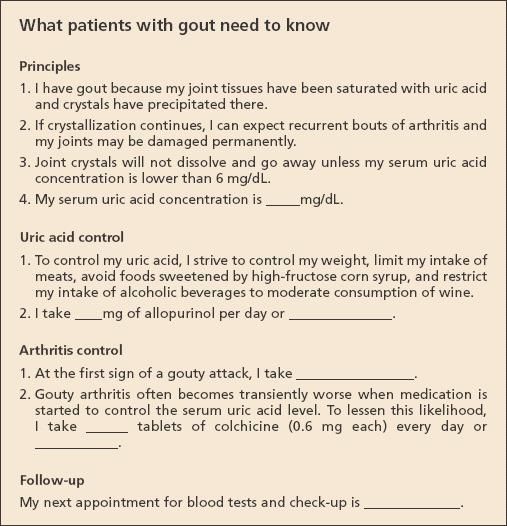
Figure
–
To help patients with gout learn what they need to know about managing their condition, physicians may provide them with a simple form such as the one shown here. The physician can duplicate the form as needed, and each patient can complete it with the physician and then hang it on the inside of his or her medicine cabinet door for easy reference.
This number is not arbitrary. It is based on the known solubility of urate in saline at 37°C (98.6°F)-about 6.8 mg/dL, the low risk of new arthritis in non-gouty patients below this level,3 and the demonstrated resolution of tophaceous deposits when hyperuricemia is controlled.4
What matters here is the long-term picture. The serum urate level often falls during acute episodes of arthritis, and low values at such times cannot be taken as evidence against gout or for effective control. Conversely, a higher value (say, about 6.4 mg/dL) may introduce an element of concern, but it need not cause a change in program for a patient who otherwise is doing well. However, sustained levels higher than 7 mg/dL imply a clear probability of ongoing crystallization, as well as the impossibility of mobilizing existing tophaceous deposits.
DIETARY CONTROL
The desire that many patients express for nonpharmacological control of their hyperuricemia deserves the enthusiastic support of all caregivers. Successful control requires exceptional commitment, but some patients say at the outset that they have little interest in a major change in their dietary ways. The most to be hoped for in these patients is progress in avoiding the most flagrant abuses, such as heavy, chronic intake of beer. In other patients, however, attention to dietary principles may play a significant-but rarely sufficient-role in the overall control of their problem. Of course, the chances are best when the hyperuricemia is modest.
Over the years, many physicians have considered purine content to be the only relevant dietary concern for patients with gout. Thus, admonitions against excessive intake of lentils, sweetbreads, and anchovies have been emphasized, but with little effect on the overall course. Purine limitation alone may induce a modest decrease in the serum urate concentration, but such restriction usually proves too unpalatable to be followed throughout a lifetime of gout.
More important than limitation of exogenous purines is a focus on factors that accelerate endogenous purine turnover. Ethanol is the most time-honored exemplar, but fructose now seems to be a more potent and more prevalent dietary concern.5,6 Both alcohol and fructose cause accelerated catabolism of purine nucleotides, ie, adenosine triphosphate. As this breakdown continues, the necessary replacement process “revs up” overall purine synthesis. The end result is an increase in uric acid production. For reasons that remain unclear, this increase in load may be accompanied by a decrease in the efficiency of uric acid excretion that compounds the hyperuricemic effect.
Among alcoholic beverages, beer is a special problem because it includes not only ethanol but also a significant purine content, unlike the distilled, “hard” liquors. Wine taken in moderation has not been found to increase either the serum urate concentration or the incidence of gout,7 perhaps because the ethanol-induced boost in synthesis is balanced by as yet unidentified uricosuric ingredients. Ascorbic acid (vitamin C) is the best-studied dietary uricosuric agent, but comparable properties are present in dairy products and coffee (consumed in generous amounts), and perhaps other “natural” uricosurics may yet be identified.
Increase seen in “metabolic syndrome”
Epidemiological surveys have found a marked (2- to 3-fold) increase in the incidence of gout over recent decades in various populations.8 The gene pool remains the same, and it seems unlikely that much of this change can be attributed to diuretics or other hyperuricemia-inducing medications. This leaves diet as the most likely cause of the upsurge, and that interpretation is supported strongly by a parallel increase in obesity, as well as other components of the “metabolic syndrome” (morbid obesity, diabetes mellitus [DM], hypertension, hyperlipemia, and gout).
If dietary change is responsible for half or more of the gout currently seen, then dietary amelioration offers the prospect of dietary control for a comparable proportion. During the endemic privation of World War II, the incidence of gout declined throughout Europe.9 Now, less stringent dietary restriction may at least serve as an important adjunct in the treatment of patients with gout.10 The most promising stratagem would seem to lie in a limitation in intake of dietary carbohydrates, with a major focus on the nearly ubiquitous high-fructose corn syrup.
Care of patients who have the metabolic syndrome now challenges clinicians in virtually every field of medicine. Gout control deserves a prominent place among the gains to be realized from more effective management of this common problem.
DIAGNOSIS
Inasmuch as confirmation of urate crystal deposition provides unequivocal confirmation of gout, many students of this disease have considered a diagnostic arthrocentesis essential in the care of every patient. In a study of diagnostic criteria, however, a group of experts undertook aspirations in only half the new patients they thought had unequivocal gout.11 In addition, when the procedure was performed, it was only about 80% sensitive.
Some patients have unequivocal tophi, and others have well-established, long-term hyperuricemia in the presence of acute peripheral monarticular arthritis. Others may have had several previous episodes that were identical to the present one and were dramatically responsive to therapy, and still others have arthritis in midfoot joints that are not accessible without fluoroscopic or sonographic guidance. In any of the patients with arthritis in midfoot joints, I would consider their problem to be gout even if I did not find the incriminating crystals. In that setting, I probably would not aspirate for diagnostic reasons, and I think that the 50% cited in the study is about right.
A difficult sell
This leaves a great many aspirations to be done, and the procedure may be a difficult sell to both the empathetic clinician and the suffering patient-particularly when the pain, like that of Thomas Sydenham (1624-1689), is such that the patient can not bear the weight of bedclothes or the jar of a person walking into the room.12 Here, the prospect of prompt pain relief provides the most telling incentive for both participants. When the patient understands that his pain is driven principally by distention of the joint capsule and the clinician understands that the same distention makes the procedure easier, both parties are more willing to proceed.
Sydenham also described a spontaneous easing of his pain after about 24 hours, and it was after this point that his foot began to swell.12 I suspect that this was the point of capsule rupture, that aspiration can provide equivalent decompression, and that the needle track serves as a vent to provide subsequent drainage. Conversely, if the pain already has eased and the foot is greatly swollen, the procedure becomes more difficult and is unlikely to relieve the pain. I would not try to persuade the patient to accept this, unless I was seriously worried about infection.
Infection
To me, infection is a special concern when significant fever or other systemic signs are present, when there are associated skin lesions suggesting a portal of entry, when the patient has DM or has other bases for immune compromise, and when the focal problem is chronic. Olecranon bursitis is a particular worry because this is a favorite target for staphylococci as well as gout. So, too, is the knee, in which infection is common and aspiration is easy.
Acute flares at these sites deserve aspiration and culture irrespective of whether crystals have been found previously because chronic gout and infection may act symbiotically. When aspiration is at issue, a physician always has time to review his thinking with the patient. If the patient thinks that the physician is trying to help his pain or is worried about possible infection, he will readily accept the procedure. If he thinks that the physician is merely curious, the trust that he has in his care may be seriously strained.
Crystal persistence
Not every patient with gout has the flagrant podagra of Sydenham. For some patients, the episodes are less disabling and last only a day or so; in addition, the episodes may be discovered only with a careful history taking, because no one of them is deemed sufficient to justify a visit to the emergency department.
If these episodes are crystal-driven, and the patient has persistent hyperuricemia, crystals will remain within the joint and their demonstration will justify urate lowering therapy. This is the setting in which intermittent episodes may evolve into a polyarticular presentation that is then mistaken for rheumatoid arthritis or psoriatic arthritis. A diagnostic aspiration is then essential to correct the misimpression and move on to appropriate treatment.
Plain radiographs indicated
In my opinion, plain radiographs of the feet (and, often, of the hands) are indicated when gout is suspected. Changes of osteoarthritis (OA) are to be expected, but a finding such as chondrocalcinosis may point in a very different diagnostic direction. Erosive lesions, cystic changes with sclerotic margins, and the classic “overhanging edge” (when bone-forming periosteum is elevated over an expanding, intraosseous tophus) all are helpful in the diagnosis of gout. When this demonstration of destruction is shown to the patient, it provides convincing evidence that his disease is not just one of periodic pain but rather one that is destroying his joints. As a result, the patient gains a powerful incentive for adherence to a regimen that may seem increasingly bothersome as the attacks become less frequent and ultimately cease.
The finding of OA also may provide an opportunity for therapeutic intervention. Many patients with OA have hallux valgus, a finding that should suggest an inspection of the patient's footwear. Pointed toes that exacerbate the valgus deformity should be avoided; a “rocker-bottom” sole may alleviate the pain and strain of hallux rigidus. In addition, a capable podiatrist may help greatly in alleviating foot problems that may exacerbate the recurrent arthritis in this classically gout-prone articulation.13
PROPHYLAXIS
In my experience, the majority of patients who think that they “cannot take allopurinol” hold this view because they tried it and their arthritis became worse rather than better. This problem arises most often in patients who have chronic tophaceous disease, and the risk continues long after the serum urate concentration has reached its target range of 5 or 6 mg/dL.
Flares occur not only with allopurinol but also with all other effective urate-lowering therapeutic agents, including probenecid, and the currently experimental agents febuxostat and PEGylated uricase. The logical and accepted explanation is that these treatment-induced episodes arise not from precipitation of new crystals but rather from the release of old crystals from tissue deposits.
Because dissolution of such deposits is a major goal of therapy, the patient must recognize the probability that flares will occur and must be forewarned and forearmed to deal with them. A well warned patient understands that flares reflect mobilization of his crystal burden and that his physician has not made an inappropriate choice. The forearmed patient is already receiving colchicine prophylaxis (usually 0.6 mg bid), although an NSAID (eg, naproxen) may be sufficient if it is already in regular use for concurrent OA. In addition to this daily prophylaxis, I think that each patient with gout also should have an extra agent on hand (a nonsteroidal agent, if the kidneys function well, or a corticosteroid, if there is renal impairment).
Gouty arthritis responds best when it is managed early. The well-informed patient, like the patient with angina or DM, should be prepared to self-treat and abort manifestations that break through the protection of daily prophylaxis.
URATE-LOWERING THERAPY
Hyperuricemia results from increased production of urate, inefficient excretion of uric acid, or both. Appropriately, then, it may be managed with an inhibitor of urate synthesis (allopurinol), a promoter of more efficient excretion (probenecid) or, rarely, both.
In the as yet unproven belief that a graduated program may induce fewer flares and facilitate recognition of rare but serious toxicity, I start allopurinol at 100 mg/d, increase it by 100-mg increments each 2 to 4 weeks, and then maintain that dose, meeting the goal of a serum urate of less than 6 mg/dL. In some patients, control is reached with 200 mg/d, but more patients require at least 400 mg/d. When there are significant tophi (and thus an increased risk of flares) or evidence of renal impairment, I start with 50 mg/d and increase by 50-mg increments.
Probably the most common error in long-term management is making the assumption that 1 dosage (300 mg/d) fits all comers. This dosage is too low for roughly half of patients with gout. Here again the patient must understand the reasoning behind this titration of daily dose versus serum response, as well as the quite different rationale for his anti-inflammatory therapy.
Probenecid
When probenecid therapy is chosen instead of allopurinol, a comparable escalating protocol makes sense. I usually start patients at 500 mg with breakfast, add a second dose with supper, and then alternate further increments at these 2 times until the serum urate level is lower than 6 mg/dL. Note that uricosuric agents should be taken with a generous intake of water and should not be taken at bedtime. This plan ensures that the expected bolus of urinary uric acid falls during periods of peak urine pH and flow rate and thus should lessen the possibility of uric acid stone formation.
Probenecid is an effective agent that would seem to be underused in contemporary American practice. When hyperuricemia is modest (and especially when it develops secondary to a morning dose of hydrochlorothiazide), a single, coincident dose of probenecid may restore a normal urate concentration. However, probenecid is ineffective in patients who have renal insufficiency (I usually do not try it unless the patient’s serum creatinine level is lower than 2 mg/dL), and it is best avoided in patients who have tophi or renal stones.
Reinforcing the essentials of treatment
Again and again physicians encounter patients who mistakenly reserve their “gout medicine” (allopurinol) for attacks and are uncertain about how or why they should take anti-inflammatory drugs. To provide reinforcement of the essentials of the treatment program and to obtain appropriate laboratory surveillance, physicians should ask even patients with well-controlled gout to return for periodic re-evaluations. In addition, patients should be advised to obtain 1 or more of the excellent patient education materials that are available on the Internet from various organizations-the Arthritis Foundation (http://www.arthritis.org), the American College of Rheumatology (http://www.rheumatology.org), and the Gout and Uric Acid Education Society (http://www.gouteducation.org).
References:
References
- 1. Hoskison TK, Wortmann RL. Advances in the management of gout and hyperuricemia. Scand J Rheumatol. 2006;35:251-260.
- 2. Choi HK, Mount DB, Reginato AM, et al. Pathogenesis of gout. Ann Intern Med. 2005;143:499-516.
- 3. Campion EW, Glynn RJ, DeLabry LO. Asymptomatic hyperuricemia: risks and consequences in the Normative Aging Study. Am J Med. 1987;82:421-426.
- 4. Perez-Ruiz F, Calabozo M, Pijoan JI, et al. Effect of urate-lowering therapy on the velocity of size reduction of tophi in chronic gout. Arthritis Rheum. 2002;47:356-360.
- 5. Choi HK, Atkinson K, Karlson EW, et al. Alcohol intake and risk of incident gout in men: a prospective study. Lancet. 2004;363:1277-1281.
- 6. Nakagawa T, Hu H, Zharikov S, et al. A causal role for uric acid in fructose-induced metabolic syndrome. Am J Physiol Renal Physiol. 2006;290:F625-F631.
- 7. Choi H, Curhan G. Beer, liquor, and wine consumption and serum uric acid level: the Third National Health and Nutrition Examination Survey. Arthritis Rheum. 2004;51:1023-1029.
- 8. Roddy E, Zhang W, Doherty M. The changing epidemiology of gout. Nat Clin Pract Rheumatol. 2007;3:443-449.
- 9. Zöllner N, Griebsch A. Diet and gout. Adv Exp Med Biol. 1974;41:435-442.
- 10. Dessein PH, Shipton EA, Stanwix AE, et al. Beneficial effects of weight loss associated with moderate calorie/carbohydrate restriction, and increased proportional intake of protein and unsaturated fat on serum urate and lipoprotein levels in gout: a pilot study. Ann Rheum Dis. 2000;59:539-543.
- 11. Wallace SL, Robinson H, Masi AT, et al. Preliminary criteria for the classification of the acute arthritis of primary gout. Arthritis Rheum. 1977;20:895-900.
- 12. Dorwart BB. Thomas Sydenham (1624-1689), on gout: 1717. J Clin Rheumatol. 2004;10:227.
- 13. Simkin PA. The pathogenesis of podagra. Ann Intern Med. 1977;86:230-233.
2 Commerce Drive
Cranbury, NJ 08512
All rights reserved.





