Article
Study Finds Time-Restricted Diets Elicit No Changes in Blood Pressure or Lipid Profile
Author(s):
A recent study found that time-restricted diets did not induce changes in blood pressure or lipid profiles, but did lead to reductions in weight loss.
This article was originally published on EndocrinologyNetwork.com.
A recent study from the Queen Mary University of London is adding to the debate around the efficacy of time-restricted eating (TRE) as an approach to cardiometabolic conditions.
A 12-week study assessing the effect of TRE in a population of obese adults, results indicate the effects were modest but appeared to be equal to those achieved with other interventions and lead investigators to call for a formal trial of the intervention.
“Simple weight management plans which people can stick to are currently lacking. In this study, more than a quarter of the participants had lost at least 5% of their starting body weight at 12 weeks,” said Dunja Przulj, PhD, a research health psychologist at Queen Mary University of London, in a statement.
With the obesity epidemic continuing to grow, a historic level of interest has been brought to dietary science and nutrition. Previous studies, conducted in animals or smaller populations, have outlined the impact of a time-restricted approach, but investigators felt these failed at accurately describing the real-world effects of TRE on weight and lipid profile among obese patients.
With this in mind, the current study was designed to restrict participants’ daily eating period to 8 hours each day over a 12-week period. During the remain 16 hours of each day, participants were permitted to drink water, diet drinks, or coffee/tea with no milk or sugar. Investigators allowed participants to choose the 8-hour period most convenient for them.
In total, 52 patients were recruited for the study through a community weight clinic and university staff bulletins and social media. All patients included in the study were aged 18 years or older, and had a BMI over 30 kg/m2 or over 28 kg/m2 with comorbidities.
Demographic data was collected from all participants at baseline. Weight was measured at baseline and at weeks 1, 6, and 12. Measurements for blood pressure and lipid profile were performed at baseline and again at 12 weeks. Adherence to the
The primary outcome of the study was adherence to TRE and secondary outcomes included drop-out rates, weight changes, changes in blood pressure and lipid profile from baseline, ratings of interventions, and others.
In total 50 patients were included in the study. These m=patients had a mean age of 50 years, and mean body weight of 97 (SD, 17.1) kg, a mean BMI of 35 (SD, 4.0) kg/m2, and 74% were female. At week 6, 64% of participants continued to practice TRE at least 5 days per week and, at week 12, 58% reported the same level of adherence.
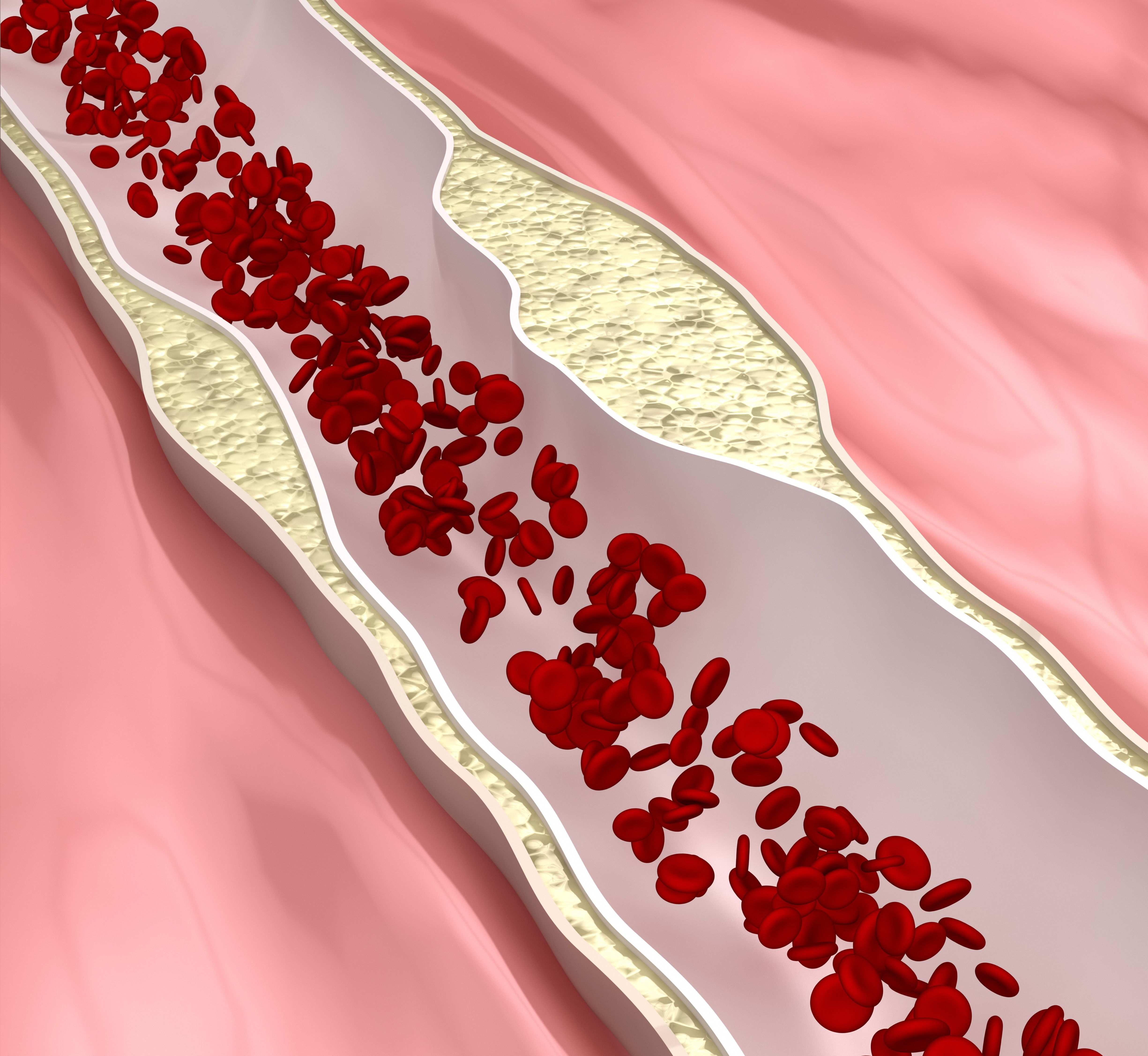
Among participants who provided follow-up data, those adhering for at least 5 days per week had greater weight loss than those with lower adherence (week 6: 2.5 [1.7] vs 1.0 [1.3], P=.003; week 12: 3.5 [2.7] vs 1.3 [2.0], P=.001). Additionally, 26% of the study sample lost at least 5% of their body weight at 12 weeks. However, investigators observed no impact on blood pressure or lipid profile.
This study, “Time restricted eating as a weight loss intervention in adults with obesity,” was published in PlosONE.





